Cataract surgery is the most common surgery performed in SNEC. This article tells you everything you need to know about cataracts and cataract surgery.

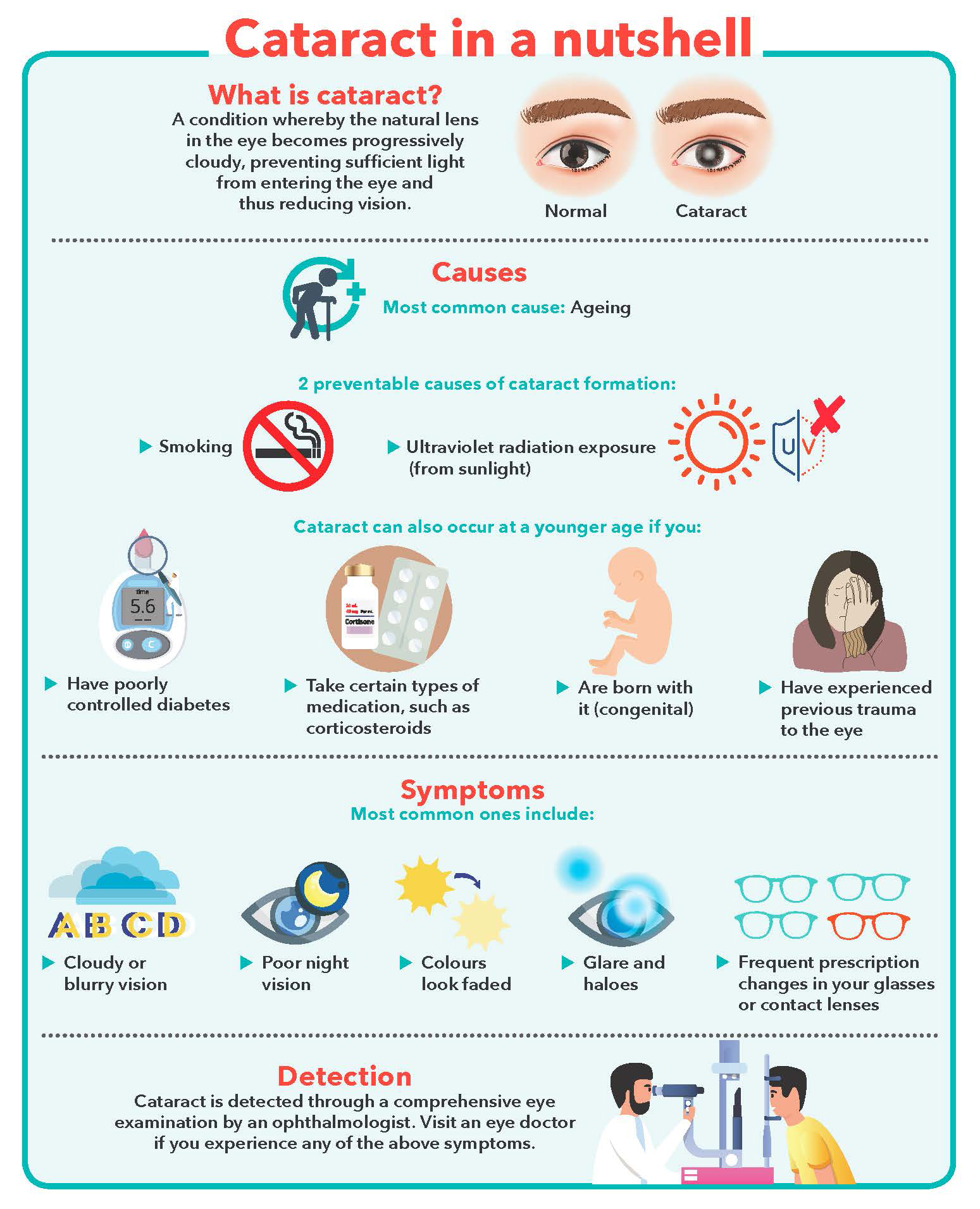
In the majority of cases, people start to develop
cataracts in their early 50s but their vision does not get affected until after the age of 60. Most cataracts develop slowly and may not be noticeable in the earlier stages of the condition.
In other cases, cataracts may be related to eye trauma, long-term diabetes, corticosteroid medications or radiation treatments.
SINGVISION speaks to
Dr Melissa Wong, Senior Consultant at SNEC’s
Cataract & Comprehensive Ophthalmology Department, to clarify common misconceptions of cataracts and understand why patients should not delay
cataract surgery amid the current pandemic.
WHEN TO GO FOR CATARACT SURGERY

Cataracts cannot be cured with medications or eye drops. Lifestyle adjustments, such as changing your spectacle lens power, using a magnifying glass to read or improving the lighting at home, can be adopted in the early stages.
When the condition starts interfering with one’s daily activities, such as driving and watching television, the cataract needs to be removed. Cataract surgery is a safe and effective procedure that is performed as a
day surgery.
At SNEC, ophthalmologists undergo strict and guided training to ensure the safety of patients. Our paramedical staff are also well trained in taking accurate eye measurements, which are crucial in obtaining good surgical outcomes. In addition, we handle complex cataract surgery in children, trauma patients, as well as those with certain congenital and medical conditions.
PREPARING FOR SURGERY
Once you have decided to do surgery, you will be advised on how to prepare for it. You will need to go for pre-operative tests within three months of your surgery date. These include the blood pressure test, urine test, electrocardiogram, blood sugar test, and eyeball length measurements.
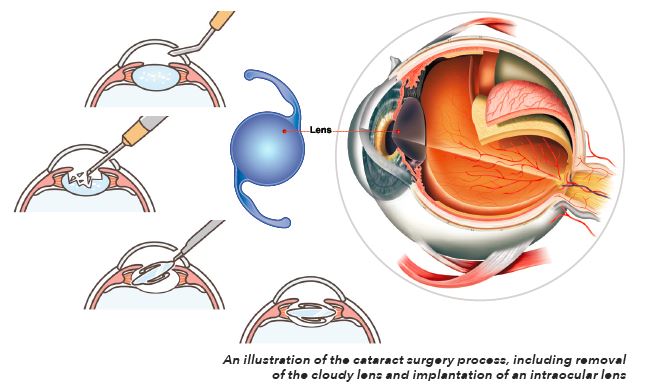
As with any surgery, cataract surgery poses risks such as infection and bleeding. You may be asked to temporarily stop taking medications that may increase the risk of bleeding during the procedure. The main technique used for cataract surgery at SNEC is phacoemulsification, in which a small ultrasonic probe is inserted into the eye via a small incision. This probe breaks the cloudy lens into tiny pieces and aspirates these fragments out of the eye. An artificial lens called an intraocular lens (IOL) is then implanted where the natural lens used to be.
“Every year, surgeons around the world introduce new surgical devices to make phacoemulsification more efficient. We have refined it with smaller wound incisions, and adopted the use of femtosecond laser,” said Dr Wong, who has been performing cataract surgery since 2007 and received specialist accreditation in 2013.
“Femtosecond laser aids in the creation of a more wellcentred capsular opening and segmentation of the cataract into many pieces. This increases the efficiency of phacoemulsification and is especially useful in the more complicated cataracts.”
Cataract surgery generally takes less than 30 minutes. An anaesthetist will be present to administer sedation. Depending on the individual, you may not be totally asleep but you will remain comfortable. Anaesthetic eye drops and injections will be given to minimise pain. It is important to avoid talking and moving your head and body during the surgery. Most of the time, the wound does not require stitching.
LENS IMPLANTS
IOLs have evolved over the years along with medical technology advancements. These lens implants are largely categorised as monofocal without astigmatism correction, monofocal with astigmatism correction (toric), and multifocal lens.
Monofocal lenses provide excellent distance vision correction but not near vision, so patients would still need glasses for near work, such as reading, after surgery.
Multifocal lenses are lenses of convenience that offer good distance, intermediate and near vision. However, multifocal lenses can cause glare and haloes, and compromise near vision in dim lighting. “I always tell my patients that multifocal lenses are not miracle lenses. They are simply more convenient with some trade-offs,” said Dr Wong.
“Newer lenses are constantly being evaluated at SNEC. There are newer multifocal lenses that allow for better intermediate and near vision without much compromise on the quality of distance vision. Currently, the latest monofocal lenses also give patients the ability to have fair intermediate vision,” she added.
POST-SURGERY CARE
After the surgery, you must keep your eye clean, wash your hands before touching your eye, and use the prescribed medications to minimise the risk of infection. Serious infection can result in loss of vision.
Cover your eye with an eye shield on the day of surgery and every night while sleeping for one week. You should also prevent contaminated water from entering the eye when cleaning your face.
Apply antibiotic and steroid eye drops as prescribed. You may experience an occasional itch, sandy feeling and/or tearing for a few days or weeks after surgery. Artificial tears can be used to relieve this sensation.
It typically takes two to four weeks for patients to recover. Any glasses required should be prescribed between three and six weeks after surgery.
Myths Debunked
Dr Wong addresses common misconceptions and frequently asked questions about cataracts and cataract surgery.
What is the biggest misconception of cataract?
Many people think that they need to wait till their cataracts are “very ripe” before opting for surgery. They believe that if the cataract is “not ripe” enough, it cannot be removed. In reality, waiting for the cataract to turn dense may cause the surgery to be potentially more complicated and result in longer visual recovery time.
Can cataract surgery be done on both eyes at the same time?
Cataract surgery itself carries a small risk of endophthalmitis (severe ocular infection), hence we strongly discourage performing surgery on two eyes simultaneously. But there are cases, such as mentally incapacitated patients who require general anaesthesia and have significant cataracts in both eyes, where we may opt to operate on two eyes at the same time.
There is no definite recommended time interval between surgeries, as this depends on the degree and density of the cataract in the fellow eye, as well as the patient’s occupation and lifestyle. If patients are able to cope with vision in the fellow eye, it is advisable to wait till the operated eye has fully recovered.
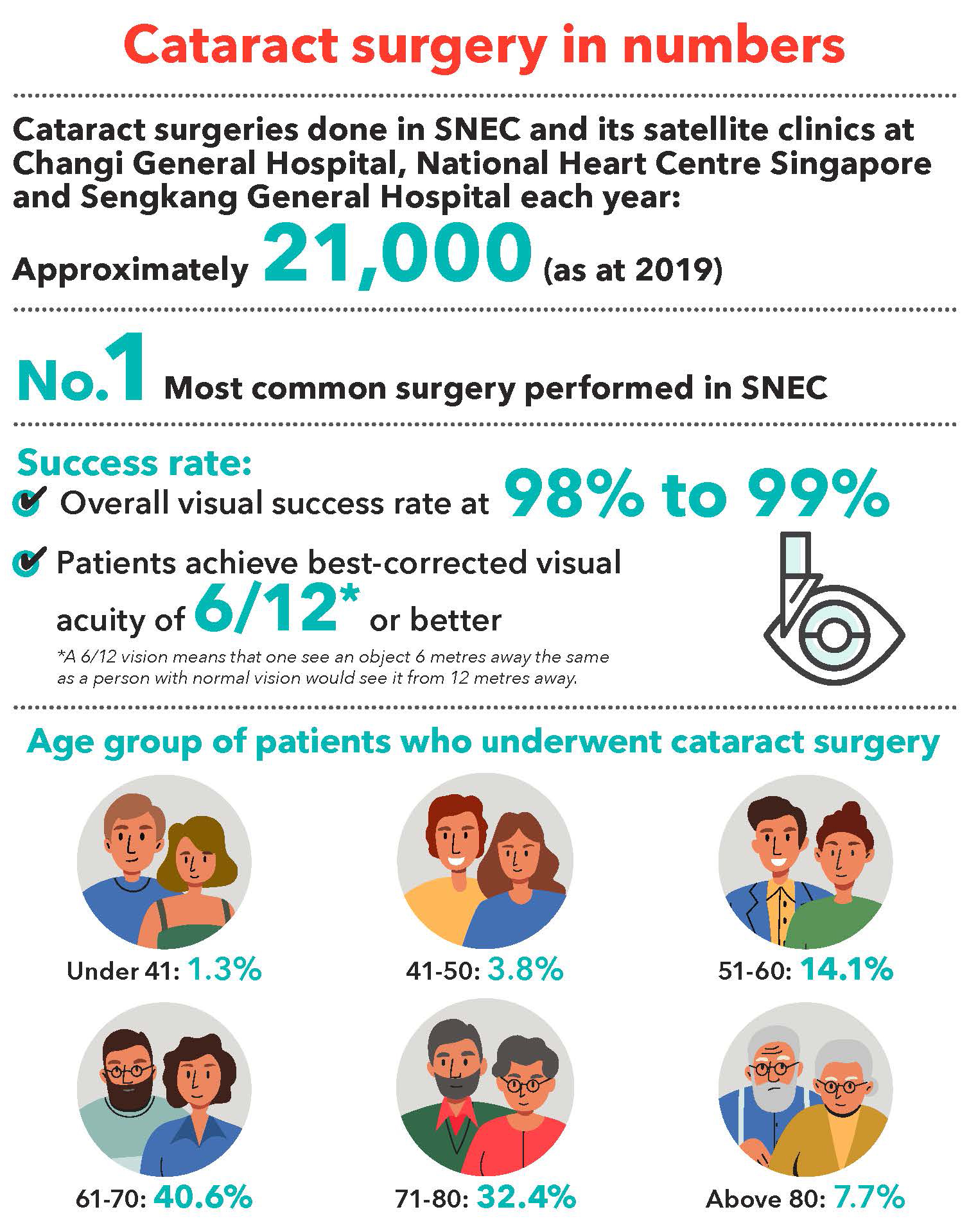
What defines a successful cataract surgery?
At SNEC, we define success as best-corrected visual acuity (BCVA) of 6/12 or better. According to our audit in 2020, 99% of our patients were able to achieve this
outcome after cataract surgery.
Personally, I feel that as long as the patient is satisfied with the result, the surgery is also considered a success. A patient with perfect vision (6/6) may not necessarily be happy due to other visual complaints, so success should not be defined by just a number; it should be evaluated based on patient feedback and their overall wellbeing post-surgery.
Can cataract surgery improve other eye conditions?
Cataract surgery with IOL implantation can almost fully correct refractive errors such as myopia, hyperopia, astigmatism, and to a large extent, presbyopia.
How long can the lens implant last? Can a cataract come back after surgery?
The IOL implant usually lasts a lifetime. After cataract surgery, it is not possible for a cataract to come back because the natural lens, which had turned yellow due to the cataract, has been removed.
However, a condition known as posterior capsule opacification (PCO) may occur three to six months after the surgery. In 20% of patients, it may happen within five years. Some people call it the “second cataract” but that is not the case. PCO happens because of the cells inside your eye that grow over the lens capsule, causing it to become cloudy. This can be resolved by a painless laser treatment called YAG capsulotomy, which takes only a few minutes to complete.
Some patients may be worried about undergoing surgery in the midst of the COVID-19 pandemic. What measures are there in place?
You can rest assured that SNEC has put its best effort into ensuring the safety of all staff and patients. Safe distancing measures remain in place across the centre, including clinics and the post-operative recovery area. We have also reduced the number of surgeries each day, as well as limit the number of accompanying persons to one per patient. If a patient is unwell, his or her surgery will be postponed.
Should patients delay surgery until after getting the COVID-19 vaccination?
No, if your vision is significantly affected, you should not defer surgery. There is no need to worry about going for cataract surgery without having had the vaccination.
Visit
Cataract & Comprehensive Ophthalmology Department for more information.
Click here to check out other articles in SINGVISION Issue 1/2021.
