Learn how SNEC’s glaucoma team enhances diagnoses, interventions, and enables patient advocacy through patient education.
Glaucoma is an eye disease caused when high fluid pressure within the eye damages the delicate fibres of the optic nerve. It is one of the leading causes of blindness in the world. In Singapore, glaucoma affects approximately 10 per cent of the population and is undiagnosed in up to 50 per cent of cases.
In its early stages, glaucoma can have little or no impact on vision, and sufferers may not have any symptoms. Glaucoma is often called ‘The Silent Thief of Sight’ since most people are unaware that they have the disease. Even when vision starts to be lost, the progress can be very slow and gradual. By the time the patient realises that something is wrong, they may have already suffered a significant amount of permanent loss of vision.
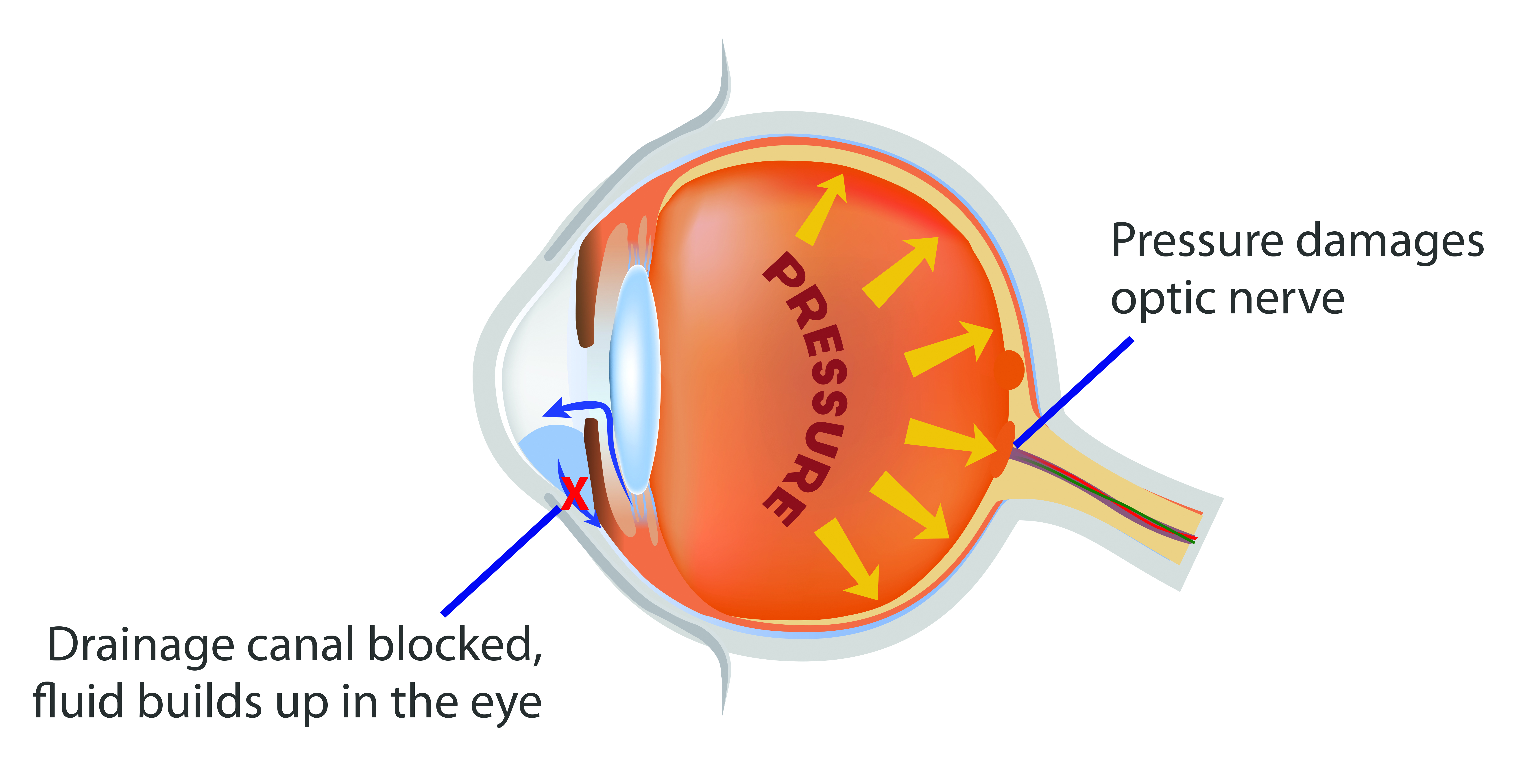
Detecting glaucoma early and implementing the appropriate treatment and education strategies are crucial for patients to preserve their remaining vision.
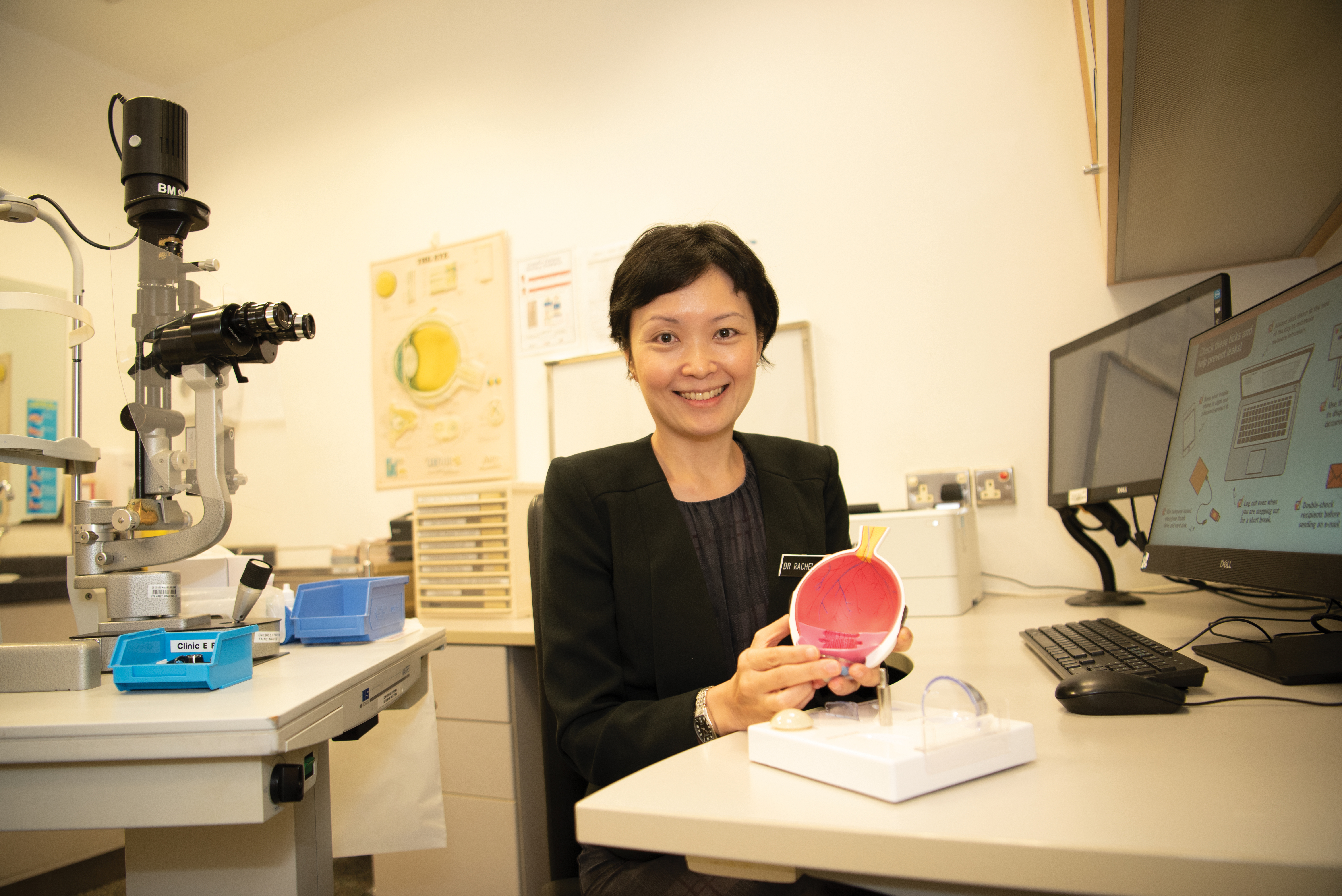
SINGVISION speaks to three doctors at Glaucoma Department — Dr Rachel Chong, Dr Olivia Huang and Dr Lee Yi Fang — to learn more about the specialised services and support available.
TREATING GLAUCOMA IN HIGH MYOPIA PATIENTS
Singaporeans with myopia, or short-sightedness, have a higher chance of getting glaucoma when they grow older and the risk increases as myopia becomes more severe, according to various studies conducted in Singapore and worldwide in recent years.
The prevalence of myopia in Singapore is among the highest in the world, with 65 per cent of our children being myopic by Primary 6, and 83 per cent of young adults being myopic. By 2050, it is projected that 80 to 90 per cent of all Singaporean adults above 18 years old will be myopic and 15 to 25 per cent of these individuals may have high myopia.
High myopia puts one at risk of many eye disorders later in life, such as glaucoma, early cataracts and macular degeneration. These complications can cause severe morbidity, even resulting in blindness.
Diagnosing glaucoma in myopic eyes is a particularly complex issue for multiple reasons. “When you have high myopia, your eyeball becomes stretched and the tissue supporting the nerve in the eye is weaker so this increases the risk of glaucoma two- to threefold.” In addition, the altered shape of the eyeball makes it challenging to interpret standard glaucoma tests originally designed for non-myopic eyes. The eye also functions differently, sometimes resembling the effects of glaucoma, rendering it difficult to make a conclusive diagnosis,” explained Dr Rachel Chong, Consultant at SNEC’s Glaucoma Department.
Myopia Glaucoma Clinic
SNEC set up a dedicated myopia glaucoma clinic with specialised eye evaluation processes within its glaucoma department in June 2020 that includes routine dilated eye examination and retinal imaging tests where needed. This subspecialty service caters specifically to patients with high myopia and glaucoma or suspected glaucoma. Since elongated eyeballs also cause retinal complications, the clinic also works closely with the retina high myopia clinic (called the myopia clinic) to provide as accurate diagnoses and treatment as possible.
Offering hope through research
According to Dr Chong, there is limited certainty on how high myopia patients with glaucoma or suspected glaucoma can be diagnosed and treated. But having confidence in identifying their condition would be immensely valuable. The myopia glaucoma clinic also continues to conduct research to diagnose and manage glaucoma in high myopia patients more effectively.
Glaucoma can only be controlled, not cured, and vision loss happens gradually over a period of time. Hence, journeying with the patients is important. “While we actively look for solutions, we want to ensure that patients are supported at every step of the way. We want them to know that losing vision does not mean losing one’s life. As their healthcare provider, we are equally invested in protecting their interests to the best of our abilities, whatever the outcome may be,” Dr Chong added.
LOW VISION AND GLAUCOMA
Patients with low vision and glaucoma also suffer from irreversible vision loss that cannot be fully corrected with glasses, contact lenses, surgery, or medications. They often experience glare and reduced contrast sensitivity in the early stages, progressing to constricted visual fields and reduced visual acuity in the more advanced stages of the disease. These affect their activities of daily living, mobility, occupation, social activities, and can also impact on their psychological and emotional well-being.
Low Vision Glaucoma Nurse Counselling Service
SNEC offers specialised low vision glaucoma nurse counselling services to help patients with low vision or at risk of low vision maximise their functionality, take care of themselves, and be as independent as possible.
Introduced in September 2021 and led by Dr Olivia Huang, Consultant at Glaucoma Department, the service fills the gap for patients who could benefit from low vision services but may not yet need an assessment by a low vision optometrist or occupational therapist. Referrals to this counselling service are made by doctors. The counselling is done on the same day after the patient’s doctor’s consult, and there is no extra charge for it at present.
Senior Staff Nurse Ivy Png, one of the trained nurses leading the nurse counselling, shared that during the session, patients will receive information about low vision, basic coping techniques, and strategies to improve their visibility.
In cases where specialised attention is required, our doctor or nurse would refer patients to the low vision team comprising optometrists, who will assess their needs and make referrals to occupational therapists and medical social workers accordingly.
Strategies to help patients live with low vision
- Increasing contrast, using devices with large keys and leveraging tactile feedback or audio devices (e.g., bump dots and talking clocks)
- Smartphone functions and phone apps which aid visibility
- Reducing indoor and outdoor glare with filters
- Visual aids like magnifiers, touch-screen braille tablets and artificial intelligence (AI) assistive technology, some of which can be browsed at and loaned from the STAAR (Smart Technology Active Ageing Resource) Corner at SNEC
- Visual skills training such as using systematic scanning strategies to avoid obstacles
- Low vision partners such as Singapore Association of the Visually Handicapped (SAVH), SPD (Society for the Physically Disabled), Guide Dogs Singapore and iC2 PrepHouse
- The OptoAid dropper that helps patients with difficulties to instil their eye drops accurately and thereby promoting compliance with treatment

The STAAR Corner at SNEC provides trial and loan service of various assistive technology devices such as magnifiers, touchscreen braille tablets and more for patients with low vision.
Coping with vision loss
With appropriate counselling and care, SNEC hopes to be able to raise awareness on low vision in glaucoma patients, in particular the difficulties they face, and how these can be alleviated by the use of adaptive strategies, visual aids, assistive technology, and caregiver training. This is so as to provide hope and support to patients who have already lost vision, or are at risk of losing vision.
“Losing vision affects simple activities and can trigger anxiety. But the support of our low vision glaucoma doctors, clinic and nurse counselling, coupled with resources and digital technology which have evolved manifold over the last five to ten years, can help patients cope and lead independent, fulfilling lives,” said Dr Huang.

ENABLING PATIENT ADVOCACY THROUGH EDUCATION
Having glaucoma or diagnosis for years does not mean a patient knows everything about the disease. It is thus important to equip patients with education and a psychosocial support network to enhance their health outcomes.
Improving health outcomes through patient education
SNEC treats patients of all ages with congenital, open, closed, and secondary glaucoma of different severities, from newborns to adults over 100 years old. It is common for these patients to have a poor understanding of their conditions due to doctors’ different communication styles and the variety of information available online. This in turn affects their compliance with medication, and can result in variable outcomes.
“Patients can benefit from education in different ways, depending on the way we present information or the time when they are ready to learn something that changes their lifestyle. Outcomes can be improved if they are empowered with the right information and resources. Our aim is to provide them just that,” said Dr Lee Yi Fang, Associate Consultant, Glaucoma Department.

“We are constantly looking into comprehensive strategies to enhance our patients’ understanding of glaucoma. Pilot projects were conducted from November 2021 to February 2022 to provide accurate, up-to-date, and accessible information to patients; 73 out of the 85 patients said they had access to educational materials.”
Some initiatives piloted were:
- Screening educational and interactive videos in the waiting areas
- Displaying informational resources such as posters and QR codes on glaucoma, low vision and common eye conditions
- Deploying service ambassadors to spread awareness about eye conditions such as glaucoma. They also helped the elderly and visually impaired use the QR codes and enable accessibility functions on their smartphones.
Such information database is crucial to make counselling more effective and enable patients to make an informed choice about their treatment with a doctor. In the long run, these would become SNEC and Singapore’s bank of comprehensive digital resources tailored to the wide needs of glaucoma patients.

Transforming patient education
The impact of physical leaflets is limited by visual impairment, literacy and language barriers. Hence, building on these initiatives, Dr Lee’s team is developing patient education videos and digital leaflets about glaucoma conditions and interventions like lasers and surgeries. In the near future, patients would be able to watch these audio-less videos in the clinic area with subtitles that can be translated into different languages. Alternatively, they could watch them comfortably at home via the SingHealth Health Buddy app, or read a printed transcript.
These resources will also transform the way patients are counselled. Doctors and nurses can play the videos while explaining their conditions and necessary procedures to the patients. The benefits and risks of the suggested interventions can also be covered in detail, customised to each patient’s needs. A visual aid would instil clearer expectations in the patients and overcome visual, linguistic and literacy hurdles.
Glaucoma Patient Support Group
To provide psychosocial care to glaucoma patients and reinforce their learning, Dr Lee started a patient support group in April 2022. Her team holds once-a-month small group sessions in a hybrid format. Here, patients with different conditions, from all walks of life share common concerns with one another and their healthcare providers. They get to ask questions outside of a consultation and speak about various things — their medical conditions, treatment options, caring for their eyes and coping with day-to-day difficulties.
The feedback received was very encouraging — all the patients are keen to learn more about glaucoma. They also want to hear about how other glaucoma patients are managing their condition and its impact on their lifestyles. Participants reported feeling cared for during the support group sessions.
Dr Lee added that in the near future, this patient support group will also get incorporated into SNEC’s new glaucoma patient referral protocol depending on their needs.
Scan the QR codes below for resources on:

Glaucoma

Low vision and assistive devices
For tips on how to prevent and manage glaucoma, click here.
Click
here to check out other articles in
SINGVISION Issue 1/2022.
