Learn how artificial intelligence (AI) is transforming eye care delivery and its role in the future of healthcare.
In an era with unprecedented availability of data, including electronic health records, wearable sensors and biomedical imaging, digital innovations like telehealth and AI systems have created extraordinary new opportunities in healthcare.
Due to the ageing population, the eye care community has seen an increase in the number of patients who require continuous treatment and management. As a result of the COVID-19 pandemic, healthcare institutions have reduced clinic sessions as part of safety measures. This has resulted in longer waiting times or even delayed treatment for patients.
AI and other digital innovations could potentially address some of the most urgent challenges facing health service providers and policymakers by fundamentally changing the screening and monitoring of diseases, enabling
more accurate profiling of disease progression, and further personalising treatment.
To learn how AI technology is redefining the way eye care is delivered, and how it can shape the future of healthcare, SINGVISION speaks to Assoc Prof Daniel Ting, Head of SERI’s AI & Digital Innovations Research Group, and Consultant at SNEC’s Surgical Retina and Cataract & Comprehensive Ophthalmology Departments.

HOW IS AI TRANSFORMING EYE CARE?
By 2050, the world’s population aged 60 years and older is estimated to be 2 billion. People are living longer, and the pace of ageing is much faster than in the past. As a result, there is a need for longer-term disease surveillance for ocular and systemic conditions like diabetic retinopathy (DR), glaucoma, age-related macular degeneration (AMD) and cardiovascular disease. Population expansion also increases the need to screen for important causes of childhood blindness, such as retinopathy of prematurity (ROP), refractive error, and amblyopia.
AI technologies can be broadly divided into eye-centric and systemic disease-centric. Eye care is an early mover in the AI field due to the availability and accessibility of large amounts of quantitative and imaging data. There has been successful clinical translation for automated analysis of retinal disease screening and cataract surgery intraocular lens biometry. In fact, AI for retinal fundal image analysis was the first United States Food and Drug
Administration (FDA)-approved autonomous medical AI system.
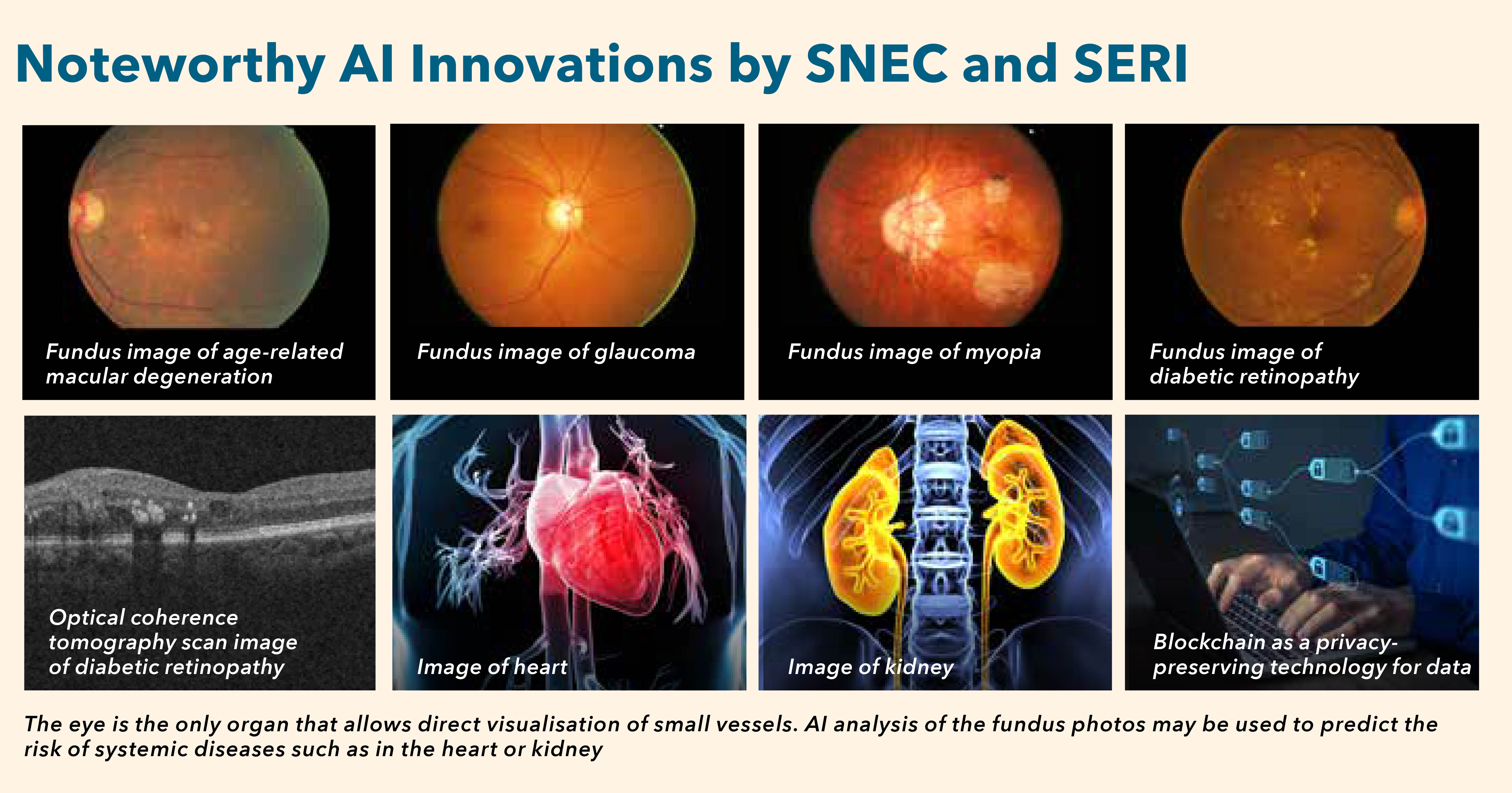
The eye is the only organ that allows direct visualisation of small vessels. Many studies are underway to determine whether major systemic issues — such as stroke or heart attack — could be predicted based on eye images, without patients needing to undergo more invasive tests, such as magnetic resonance imaging and diagnostic angiograms.
If proven to be successful, these AI developments have the opportunity to clinically transform the way eye care and healthcare is delivered.
SNEC & SERI’S AI INNOVATIONS
At SNEC and SERI, our venture into AI technologies started in 2014.
To date, SERI’s AI Programme has garnered over $20 million in cumulative grant funding. The team has also written more than 50 papers on AI that were published in renowned medical journals, including
The New England Journal of Medicine, The Journal of the American Medical Association, Nature Medicine, Nature Biomedical Engineering, The Lancet Digital Health, and more.
Most of the AI technologies developed by SNEC and SERI have undergone robust clinical validation using different well-curated clinical data sets from local andinternational collaborators.
Next steps
- Real-world clinical adoption and digital integration of mature AI projects to benefit the local and global populations
- Explore different commercial strategies to generate a sustainable return of investment in the AI technologies developed by SNEC and SERI, which can be channelled back to fund and support more AI innovations within SingHealth and Duke-NUS
SELENA+ (Singapore Eye Lesion Analyser Plus)
This AI system is focused on using retina colour photos and deep learning to detect three major blinding conditions — DR, AMD and glaucoma. In collaboration with NUS School of Computing, SNEC and SERI have jointly developed and tested SELENA+ in over 10 multi-ethnic data sets. With SELENA+, patients can obtain results within minutes rather than at least a day. SELENA+ has received regulatory approvals in six countries and is licensed for use in more than 20 countries via a spin-off company called EyRIS. It is currently integrated into the national DR screening programme, and included as part of the Smart Nation and Digital Government Office’s National AI Strategy in healthcare.
SIVA-DLS
SNEC and SERI have also worked with NUS School of Computing to further develop other AI technologies, including the SIVA-DLS (automation of retinal vessels analysis to detect cardiovascular disease) and a system to detect chronic kidney disease.
The models performed comparably to or better than expert graders in associations between measurements of retinal-vessel calibre and cardiovascular disease risk factors. Additionally, we are partnering international
collaborators to develop an AI algorithm that is effective in predicting coronary artery calcium score based on fundus images.
Fundus-based algorithms
We are partnering A*STAR on various AI projects, including:
- Using fundus photos to detect patients with papilloedema, a potentially life-threatening condition
- A fundus-based algorithm to detect patients with visual impairment, which could be utilised for population-based screening
- An AI system using colour fundus photos that is clinically effective in detecting patients with high myopia and myopic macular degeneration
- Using blockchain to govern data and the transfer of the fundusbased AI model, and ensure transparency in reporting of the AI diagnostic performance
BENEFITS OF AI ADVANCEMENTS
AI technology can be leveraged to bring about positive changes for both patients and healthcare professionals.
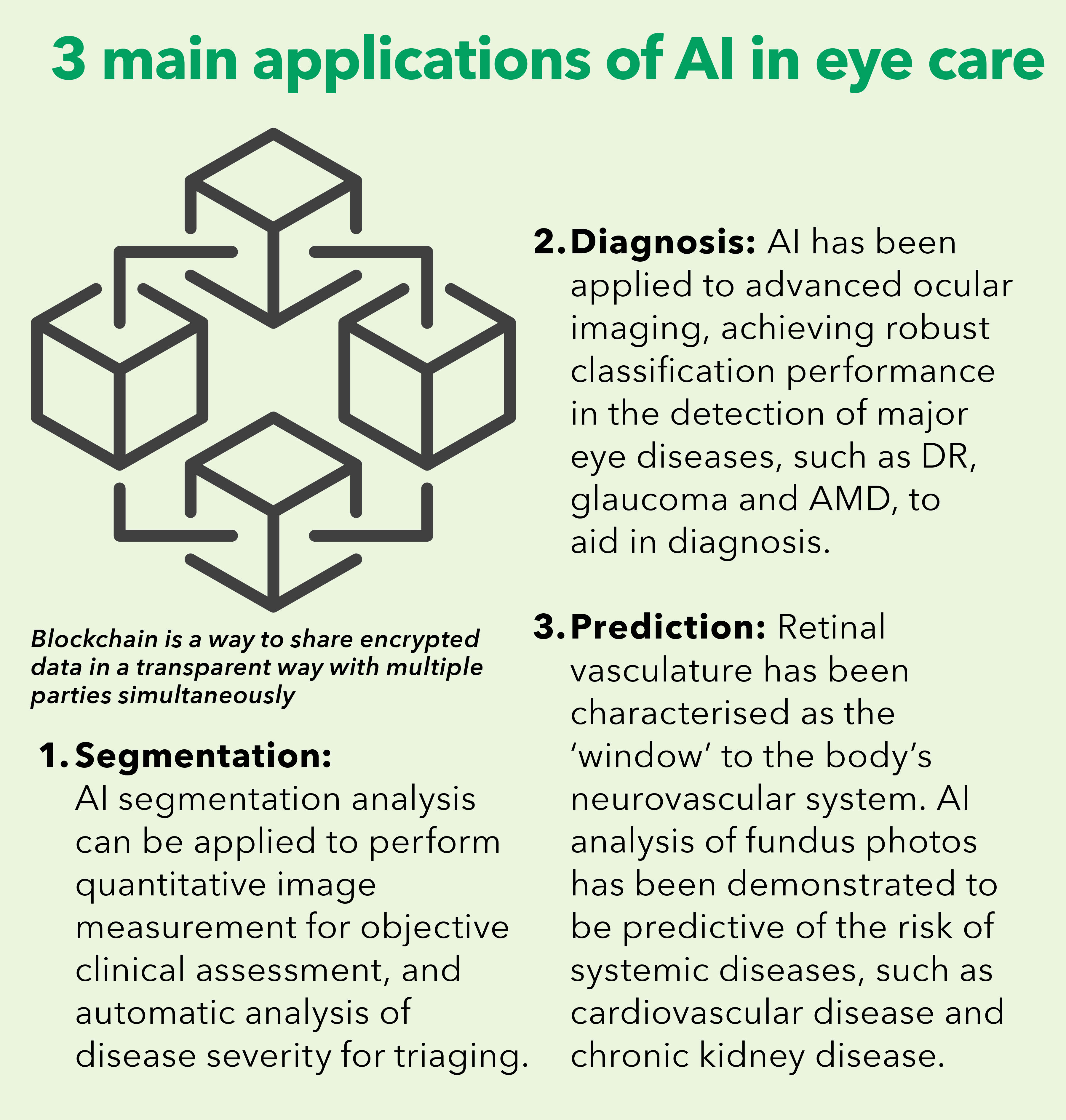
Minimise manpower requirements
AI elevates automation, which in turn reduces manpower constraints. AI can help reduce the workload of healthcare workers, and even provide medical expertise when there is shortage of medical practitioners. For example, an AI system can analyse fundal images much faster, at a rate that is unmatched by manual labour. Increasingly, AI will avail human graders from the repetitive task that involves differentiating urgent and stable eye conditions based on clinical data or eye images. It is, however, important to note that the deployment of such AI technology requires careful planning, infrastructure, and specialist support.
Improve efficiency and accessibility
AI enables more efficient diagnosis and remote monitoring, which allows for the shifting of care from the hospital to community. Resources can be more evenly distributed, translating to lower costs for patients, decreased waiting
times, and increased accessibility. Reducing the strain on tertiary eye centres will lead to an overall improvement in the quality of care provided to patients.
Improve clinical outcomes and accuracy
AI can be used to improve clinical outcomes (such as greater accuracy in post-cataract surgery refractive outcome), and reduce errors (such as active detection of medication dispensing errors).
Support clinical decision-making
In the future, AI could form the foundation of predictive and personalised eye care. This means that patients at higher risk of disease manifestation or progression can be identified and treated early. Such information would help the ophthalmologist formulate his management plan and support his decision-making, ultimately culminating in better patient care and treatment outcomes, reduced healthcare costs, and higher quality of life for the patient.
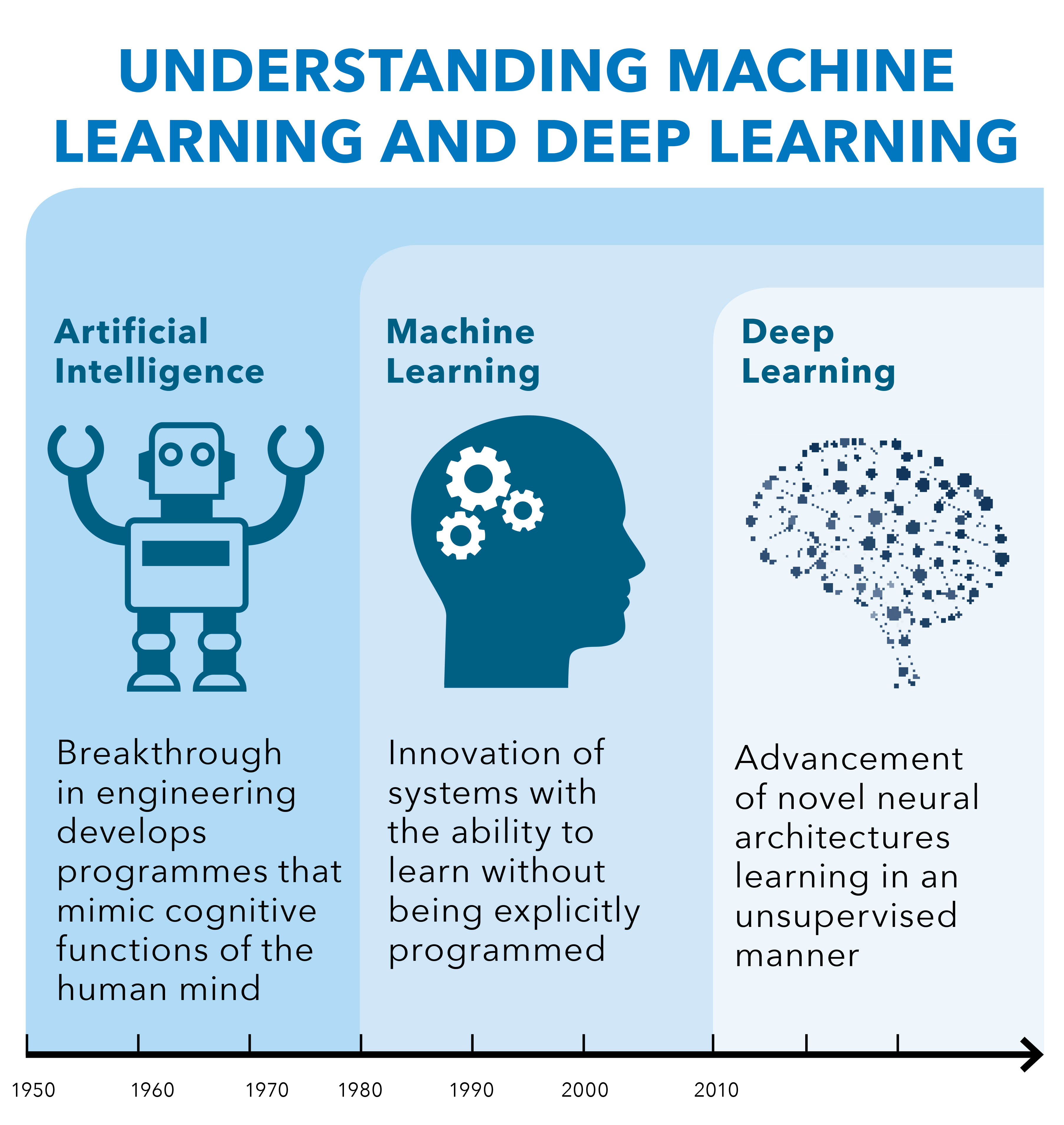
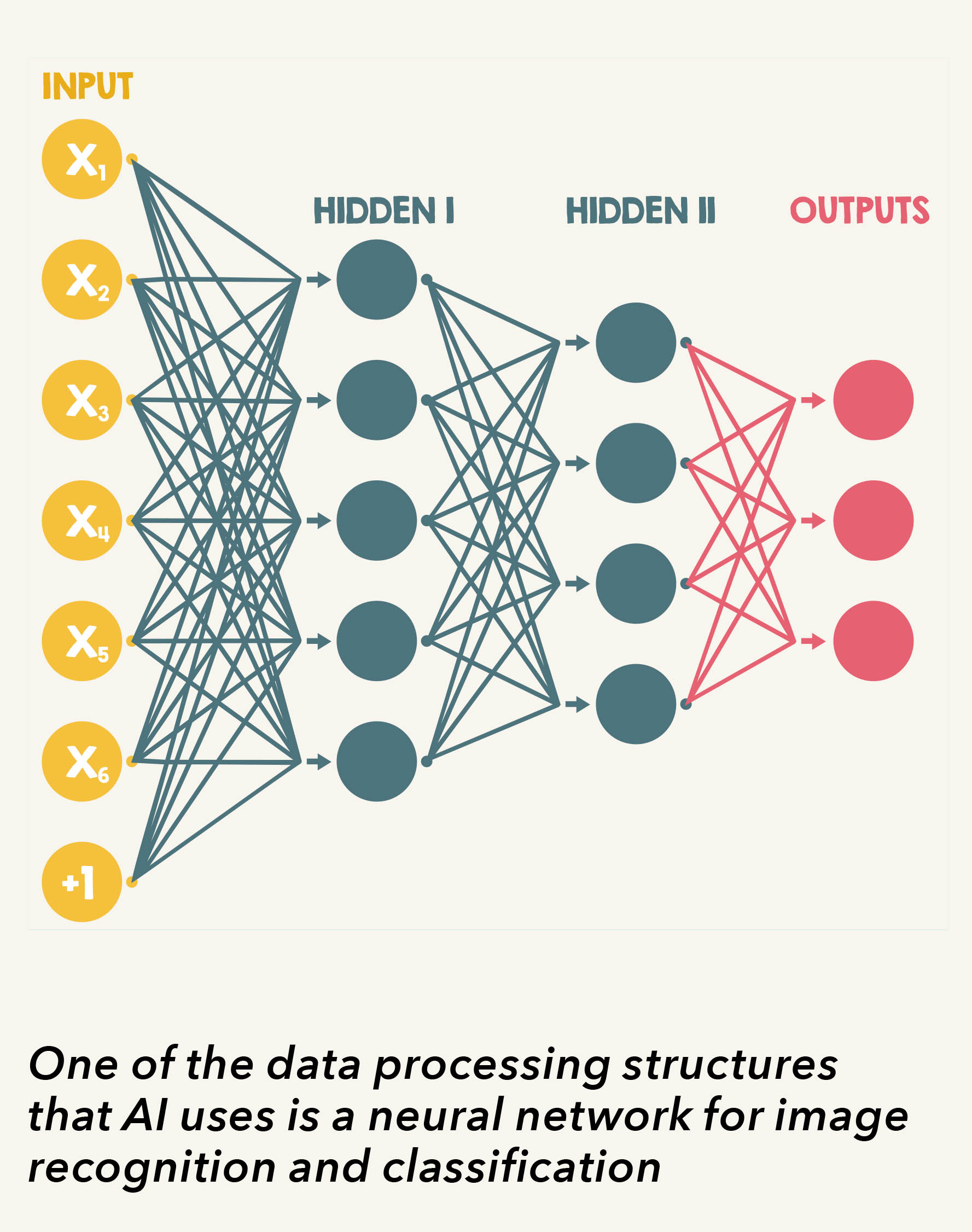
AI was first conceptualised in 1956, after a workshop at Dartmouth College in the US. The term ‘machine learning’ (ML), coined by Arthur Samuel in 1959, is defined as “the computer having the ability to learn using various statistical techniques, without being explicitly programmed”. ML algorithms can learn and make predictions based on the data that has been fed into the training phase, using either a supervised or unsupervised approach.
A part of the ML family, deep learning (DL) is based on artificial neural networks with representation learning. The ML algorithms in DL utilise multiple layers to progressively extract higher-level features from the raw input. For example, in image processing, lower layers may identify edges while higher layers may identify the concepts relevant to a human, such as faces. DL is now widely adopted in image recognition, speech recognition, and natural language processing.
ALLAYING CONCERNS
It is understandable that innovations, without traditional human contact, may not be readily acceptable by the older generations, who are accustomed to conventional healthcare models. However, these rapid advancements are supported by scientific evidence — AI platforms undergo vigorous evaluations with external testing data sets to ensure accuracy and safety, and that the robust results are reproducible. In addition, regulatory approvals from health authorities, such as the FDA and Health Sciences Authority (HSA), also attest to the technology’s efficacy.
With the COVID-19 pandemic, the world has undergone significant digital transformation that also impacts the elderly population. In fact, the crisis has catalysed the adoption of digital and AI solutions in our day-to-day
lives, resulting in increased acceptance of digital utilisation across all age groups.

THE FUTURE OF AI TECHNOLOGY
It is important to assess the technical methodologies, clinical characteristics, and cost-effectiveness of the AI system when integrated into the real-world setting. Currently, SNEC and SERI are evaluating the clinical adoption, health economic analysis, and service outcomes of the AI algorithms developed over the past few years. Apart from retina and glaucoma projects, the teams are also venturing into projects in myopia, cornea, refractive, contact lens, cataract, and intraocular lens.
To facilitate cross-border data sharing and collaborations, SNEC and SERI are also exploring various privacy-preserving domains, such as blockchain, federated machine learning, and continual learning approach. At the same time, our AI laboratories are looking into other domains, including natural language processing for conversational AI projects, such as chatbots, to promote health education, improve clinical workflows, and enhance patients’ experience in the healthcare system.

“SNEC and SERI have a diverse team of clinicians and scientists, and predecessors who have put great effort to build and establish the highly valuable clinical programmes and data sets that enable AI projects,” said Assoc Prof Ting.
“Without that, our AI teams would not have progressed as fast. This also highlights that we have to maintain strong collaborations with each other, so we can continue to lead in the AI innovation space in Singapore and globally.”
This article was contributed by Assoc Prof Daniel Ting, Dr Ng Wei Yan and Dr Gilbert Lim.
Click
here to check out other articles in
SINGVISION Issue 2/2021.
