Singapore National Eye Centre will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Research: Differences in optic nerve structure and function - normal vs high tension glaucoma
- Educating to improve patients’ compliance to intravitreal injection therapy
- I-hear-you: A Dayward Nurses Kaizen project
- Research: Using AI to screen for visually significant cataracts in the primary health care
- Research: SERI’s partnership with University College London
- Research: Real world evidence in AMD treatment
- Education: Collaborating with Vietnam National Eye Hospital (VNEH)
- Education: SNEC-GO Webinar
- SNEC/SERI Awards (April – September 2022)
- SNEC Nursing awards 2022
- SNEC’s contributions to Singapore Allied Health Conference 2022
- Psychological effects of strabismus
- Day in the life of a Low Vision Optometrist
Glaucoma is a major blinding disorder and is defined by cell damage at the back of the eye within a fragile structure known as the optic nerve head (ONH). When cells are damaged, visual information cannot reach the brain, and the patient is declared legally blind from glaucoma. To date there is consensus that glaucoma is a mechanical disorder, meaning that a given ONH exhibiting ‘fragile’ behaviour (in response to intraocular pressure, cerebrospinal fluid pressure, or gaze-induced optic nerve traction) may be at higher risk of damage. However, up until now, no tests or technologies have yet been provided to test such an hypothesis.
In a recent study led by Assoc Prof Michael Girard and Dr Thanadet Chuangsuwanich, the authors developed custom AI&Engineering tools – after a 10-year effort – to provide a comprehensive assessment of the biomechanics of the ONH in a large population of glaucoma patients for the very first time. When such tools were combined with 3D medical imaging (known as optical coherence tomography or OCT), the authors were able to: (1) map in vivo local ONH deformations (in response to an acute – but safe – increase in eye pressure); and (2) identify associations between ONH deformations and measures of blindness (ass assessed clinically). The authors found that the glaucoma eyes that exhibited the most deformations were also the eyes that were the most blind. This was true for one type of glaucoma (known as high-tension glaucoma) but not for another (known as normal tension glaucoma), which could suggest a distinct pathophysiology between these two major glaucoma sub-types.
Overall, this study is exciting because it highlights the potential role of biomechanics in glaucoma pathogenesis, and the fact that different glaucoma sub-types may benefit from different treatment options. Since this cohort of patients will be followed longitudinally, the authors will have an opportunity to identify the main mechanical factors that could ultimately lead to blindness in those patients, so as to provide earlier and personalised interventions.
Paper reference : https://www.sciencedirect.com/science/article/abs/pii/S0161642022006224
https://www.biorxiv.org/content/10.1101/2021.12.15.472712v2
For more information, watch this video as Assoc Prof Michael Girard discusses on his research work:
Internet access required
Questions & Answers for Video Interview with Assoc Prof Michael Girard:
Can you give us a brief idea about your study and its primary objective?
Our goal was to study the relationship between Optic Nerve Head (ONH) biomechanics and visual field loss in Normal Tension Glaucoma (NTG) and High Tension Glaucoma (HTG) subjects.
What is the fundamental difference seen in patients with high tension glaucoma and normal tension glaucoma patients and what did you want to compare between these subjects? (can explain the design of the study here)
We wanted to identify links between biomechanics and visual field loss in these 2 glaucoma subtypes, and whether there would be differences. For this study, we set up the largest biomechanical cohort of glaucoma patients worldwide. All patients (n>200) underwent biomechanical testing to assess the robustness of their ONHs.
What are the key takeaways of your study?
We found that a higher level of ONH deformation (due to an acute change in Intraocular Pressure (IOP) through a biomechanical stress test) correlates with higher visual field loss in HTG subjects. But this was not true in NTG subjects.
Why is this study so significant?
We still do not know why glaucoma could occur at normal levels of IOP, and this is basically what is happening in NTG patients. Our data basically suggest a distinct pathophysiology between the 2 glaucoma subtypes. Some eyes maybe more sensitive to some loads and not others. This is only the beginning of the story, but we are now quite confident that biomechanics is a critical element that will allow us to better understand, diagnose, and cure glaucoma. In addition, all patients are currently being followed longitudinally, and we will be able to report in 2-3 years on how biomechanics could help us predict visual field loss progression.
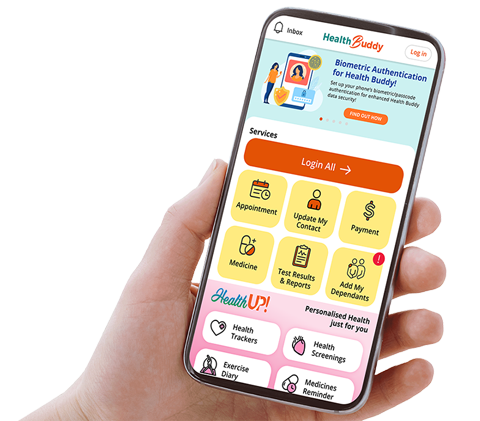
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.