Singapore National Eye Centre will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Uveitis post COVID-19 vaccine
- The Role of an Ocular Brachytherapy Nurse
- Using AI to predict high myopia risk in children
- Research: Role of HDL3 cholesterol in primary open-angle glaucoma
- Research: Improving OCT assessment in early glaucoma
- Education: SNEC’s MOU with the Institute of Adult Learning (IAL)
- SNEC / SERI Awards (October 2022 – March2023)
- Research: SERI and NTU collaboration in developing ocular imaging technologies
- Education: Experiences from a Paediatric Retina fellowship
Vaccine-associated uveitis is a known rare adverse event that has been previously described following other common vaccinations. The unprecedented nature of the Coronavirus (COVID-19) pandemic has led to the rapid development of COVID-19 vaccinations which are safe and effective. However, vaccine-associated uveitis has been also reported after COVID-19 vaccination. Concerns over the waning effects of the initial COVID-19 vaccination have led to national vaccine booster campaigns advocating the bivalent vaccination to boost humoral response. Due to the scale of these COVID-19 national booster campaigns, patients who have experienced vaccine-associated events after their initial vaccination are often anxious about booster-related flares.
We reported a low (1.39%) incidence of COVID-19 vaccine and booster related uveitis in the Singapore National Eye Centre (SNEC). These patients developed uveitis within 14 days after undergoing COVID-19 vaccination (primary and/or booster). They presented with blurring of vision, red eye and eye pain (Table 1). None of our patients developed systemic diseases or sequalae. Fifty percent of them presented as a non-infectious anterior uveitis (NIAU) (Figure 1A), while the remainder presented with a reactivation of an underlying latent infection. Our study found that the anterior uveitis was self-limited in nature, responsive to corticosteroids, which were tapered over 1-2 months, and did not result in systemic sequelae. For the infectious uveitis, they responded well to appropriate antimicrobial therapy with complete resolution, and remained well and quiescent after cessation of therapy.
For patients, with NIAU, as with any uveitis, the management of COVID-19 vaccine-related uveitis is a diagnosis of exclusion, and thus the identification of an underlying etiology with the exclusion of infections remains important. Apart from the standard uveitis questionnaires for previous uveitis, medical history and constitutional health symptoms, during the COVID-19 pandemic, vaccination status and past COVID-19 infection history are additional questions that clinicians should enquire about. Appropriate definitive treatment is essential for the fast resolution of uveitis symptoms and visual recovery.
For the non-uveitis trained ophthalmologist, the presence of granulomatous keratic precipitates (KPs) (Figure 1B) should alert the individual to exclude infective causes, rather than presume that all vaccine-related uveitis is immune-mediated. For a latent viral reactivation (specifically for varicella-zoster and cytomegalovirus), it has been postulated to be related to the robust T-cell response following vaccination which causes a massive shift and increased CD8+ T cell and T-helper type 1 (Th1) CD4+ T cells specific for the spike protein or other antigens of SARS-CoV-2. This can lead to a paradox of VZV or CMV-specific CD8+ cells temporarily unable to control the latent virus, and hence precipitating a reactivation.
The role of prophylactic treatment prior to future covid-19 vaccination booster remains undetermined given the low incidence of vaccine-related uveitis. Our experience reflects our patients’ concerns, that it may have a role in alleviating the stress addressing vaccine and booster hesitancy. Our patients expressed anxiety at the potential recurrence of visual loss when it was time for the booster and requested prophylactic therapy. In our series, our patient with ocular toxoplasmosis was prescribed prophylactic trimethoprim-sulfamethoxazole as the loss in vision during a flare was significant and she did not experience a recurrence with the booster vaccination. Patients with CMV and VZV uveitis respectively were also prescribed prophylactic antiviral therapy at the time of their booster and did not report any uveitic flare. However, it should be emphasized that the risk and benefits of such prophylactic therapy should be discussed with the patients since the incidence of vaccine-related uveitis is low.
In summary, we reported a series demonstrating the clinical spectrum of COVID-19 vaccination-induced uveitis, with majority being self-limiting, with good responses to treatment and no long-term sequelae. With COVID-19 becoming endemic, booster bivalent COVID-19 vaccination may still be occasionally required in high risk individual and thus it is important for ophthalmologists and generalists to be cognizant of COVID-19 related uveitis and advise patients accordingly as the benefits of COVID-19 vaccination and booster still outweigh the risk of uveitis.

Figure 1A: Non-Infectious Anterior uveitis with fine diffuse Keratic Precipitates
Figure 1B: Granulomatous keratic precipitates

Figure 1C: Reactivation of Toxoplasma Chorioretinitis after COVID-19 vaccination
Figure 1D: Resolution of Toxoplasma Chorioretinitis with treatment

Table 1: Patient clinical findings, treatment, and outcome of COVID-19 associated uveitis

Image and paper source:
https://www.frontiersin.org/articles/10.3389/fmed.2022.925683/full
Contributed by:

Dr Milton Chew
Associate Consultant
Ocular Inflammation & Immunology Department
Singapore National Eye Centre

Dr Anita Chan
Head & Senior Consultant
Ocular Inflammation & Immunology Department
Singapore National Eye Centre
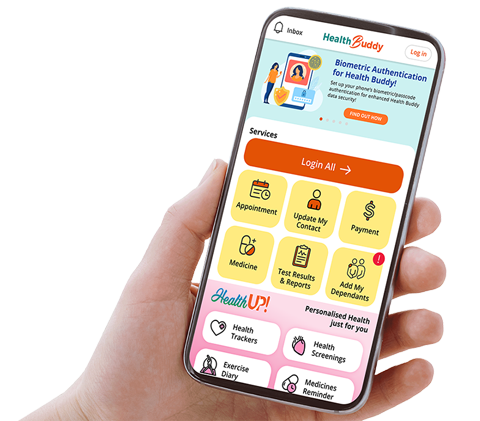
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.