Singapore National Eye Centre will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Optic neuritis: an Asian perspective
What is optic neuritis?
Optic Neuritis (ON) is a condition where inflammation of the optic nerve which connects our eye to the brain. Due to the Inflammation the nerve stops working and this results in blurring or complete loss of vision. In many cases there is spontaneous recovery but in some severe cases the loss of vision can be permanent.
Isn’t optic neuritis usually seen in patients with multiple sclerosis?
That is true. In most parts of the world optic neuritis is associated with a condition called Multiple Sclerosis (MS). Optic neuritis due to MS is usually mild and in most cases recovers spontaneously. Since the condition is so common, most studies on optic neuritis have involved patients with MS and current treatment protocols are governed by how patients with MS respond. However, in recent years there have been increasing numbers of severe optic neuritis cases where standard treatment protocols were ineffective.
Why are severe cases of optic neuritis different? Are they just severe MS?
The Mayo lab in the United States tried to answer this question by studying the blood samples these patients with severe optic neuritis and found that majority of patients with severe optic neuritis tested positive for an antibody in their blood called the Neuromyelitis Optica (NMO) or the Aquaporin 4 (AqP4) antibody. The presence of this antibody predicted severe and recurrent optic neuritis and ‘NMO spectrum disease’ is now a well-recognised condition responsible for severe optic neuritis.
Is NMO related optic neuritis also a disease more common in Europe and America like MS?
NMO antibody testing became available in Singapore 8-10 years ago. Since then, by testing all our patients with optic neuritis patients for NMO antibody, we have discovered that NMO associated optic neuritis is much more common in our population than in other parts of the world. We have also discovered that locally, more cases of optic neuritis are associated with NMO than with MS.
MS usually occurs in young patients. Is NMO also more common in the young?
Our studies have shown that unlike MS associated optic neuritis which commonly occurs in younger patients; NMO associated optic neuritis occurs in older patients as well. In our population, we have seen patients over 50-60 years of age with NMO.
What warning signs should one look out for that might suggest an episode of optic neuritis?
In a patient developing optic neuritis there is often blurring or darkening of central vision in one eye which progresses over a few days. It may be associated with pain on moving eyes or a headache. Other neurological symptoms like vomiting, imbalance or limb weakness may suggest additional brain and spine involvement.
Given this new knowledge on NMO optic neuritis, what is the best immediate course of action if one sees a patient with these symptoms?
Unlike MS optic neuritis, patients with NMO optic neuritis have poorer prognosis. They need urgent evaluation and treatment to improve visual outcomes. Therefore these patients should be referred urgently to a neuro ophthalmologist or neurologist. They will require a clinical evaluation of the optic nerve (poor colour vision, pupil reaction with or without optic disc swelling (Fig 1) followed by an urgent MRI of the brain and anterior visual pathway with contrast to look for selective enhancement of the optic nerve (Fig 2). They will also require blood tests to evaluate their suitability for systemic steroid therapy. In addition, they will be tested for presence of NMO antibodies in their blood. This test is now routinely available in Singapore, and can be ordered through the National Neurology Institute (NNI).

What treatment can be given for NMO optic neuritis and do these patients go blind?
In most cases, patients are admitted for daily intravenous steroid infusions for 3-5 days. If unresponsive to this, additional immunosuppressive treatments such as plasmapheresis or Intravenous Immunoglobulin (IVIG) may be administered. Patients are then discharged with oral immunosuppressive therapy to be continued at home. Unlike MS patients, those with NMO require longer and sustained immunosuppressive treatments to prevent future relapses. Overall, while the likelihood of complete blindness in both eyes is low, even with aggressive treatment there are some cases where complete blindness can occur. It is therefore important to be aware of and suspect NMO optic neuritis early and refer these patients appropriately, particularly given the relatively higher prevalence of the condition in our population.

Contributed by:
Dr Shweta Singhal
Consultant
Neuro-Ophthalmology Department
Singapore National Eye Centre (SNEC)
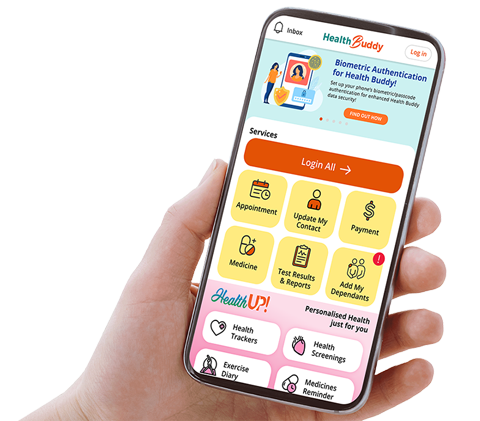
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.