Singapore National Eye Centre will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Fellowship in Oculoplastic Orbital & Lacrimal-surgery
Objective
The SNEC Oculoplastic, Orbital & Lacrimal Surgery Fellowship programme provides advanced training in the medical and surgical aspects of diseases of the ocular adnexae, orbit and lacrimal system. The programme also offers opportunities for exposure to peri-ocular aesthetic procedures and surgeries.
Duration
1 year
Programme Details
Clinical Exposure
Fellows will be rotated through the Oculoplastic and general clinics which are run by different consultants of the faculty. A wide-ranging spectrum of conditions will be encountered. The fellow is expected to be well-versed in all of the topics and skills listed below to play an active role in the delivery of care for the patients:
General Knowledge
Anatomy and physiology of the orbit, eyelids, lacrimal system, nose, sinuses, and head and neck as it relates to the orbits and adnexa
Principles of plain films, computed tomography, magnetic resonance imaging and ultrasound imaging relating to the head and neck with particular emphasis on the orbit
The appropriate imaging to order, given the clinical setting, and the ability to interpret the scan results
Eyelids
Diagnostic evaluation of eyelid malpositions (dermatochalasis, ptosis, entropion, ectropion and eyelid retraction)
Eyebrow position assessment for brow ptosis and paralysis, determining its relation to upper eyelid dermatochalasis and blepharoptosis. Evaluation of the effects of mid-face cicatricial, paralytic and involutional changes on the lower eyelid position
Assessment and management of childhood ptosis
Evaluation of eyelid neoplasms and principles of eyelid oncologic surgery and reconstruction after clearance
Regional anatomy including frequently used graft donor sites such as auricular cartilage, hard palate, buccal mucosa, posterior auricular and supraclavicular skin
Facial flaps for functional correction related to the management of periorbital malignancy
Eyelash abnormalities (trichiasis and distichiasis)
Lacrimal
Evaluation of the patient with tearing
Principles for lacrimal procedures, including external and endoscopic dacryocystorhinsotomy, canalicular reconstruction, conjunctival-DCR with Jones' tube placement
Understanding nasal endoscopy as related to the management of lacrimal and periorbital processes
Understanding sinus surgery and endoscopy as related to periorbital and lacrimal processes
Orbit and Socket
Common orbital problems of children including orbital cellulitis, benign and malignant tumours and congenital anomalies
Common orbital disorders of adults including orbital cellulitis, thyroid orbitopathy, idiopathic orbital inflammation, vasculitis, congenital tumours, vascular tumours, neural tumours, lacrimal gland tumours, fibro-osseus tumours, histiocytic diseases, lymphoid tumours and metastatic tumours
Different orbital approaches for exploration, biopsy and tumour excision
Orbital trauma including the technique of orbital floor fracture repairs and the use of different orbital barrier implants
Indications for an evisceration, enucleation and exenteration
Management of the anophthalmic socket
Aesthetics
Concept of the face as a combination of individual harmonious aesthetic units and their inter-relationships to each
Fundamentals of peri-ocular cosmetic surgery and its complications with emphasis on the upper and lower eyelids, brows and mid-face
Use of neuromodulators (botulinum toxin) and dermal fillers for the management of skin contour abnormalities. Botulinum toxin is also used widely in the centre for functional improvement in patients with blepharospasms and hemifacial spasms
Principles of filler use for periorbital rejuvenation and orbital rehabilitation, including orbital volume replacement, eyelid malposition and periorbital volume deficiency
Principles of autologous fat grafting for orbitofacial volume restoration
It is the responsibility of the fellow to review all patients daily on the ward and be involved in their day-to-day management. He/she should actively participate in the post-operative care of surgical cases in which he/she will be part of the surgical team. This will play a big part in the fellows’ learning.
The fellow is the first port of call for all Accident & Emergency patients after hours every day. Together with the consultant, the fellow will be expected to perform the initial assessment and institute treatment for all acute cases.
Surgical Exposure
The fellow will be attached to a consultant in the operating theatre for all sessions. For most oculoplastic and lacrimal procedures, he/she will first observe and assist a minimum number of surgeries before proceeding to perform them under supervision. He/she will only be assisting or performing a part of the surgery for the majority of the orbital cases. For aesthetic cases, the fellow may only assist
The fellow is strongly encouraged to practise the basic suturing techniques outside of the operating theatre, leaving valuable operating theatre time for the acquisition of more advanced skills
Minor surgeries and practical procedures can also be performed by the fellow in the treatment room at the end of each clinic session
Educational / Research Exposure
Fellows are required to participate in clinical rounds and daily ward reviews, journal clubs/teaching programmes, retrospective and prospective clinical research and quality assurance audit programmes of the department. All fellows will also participate in teaching of residents and/or medical students and attend all SNEC meetings.
Number of Places Available
2 every year
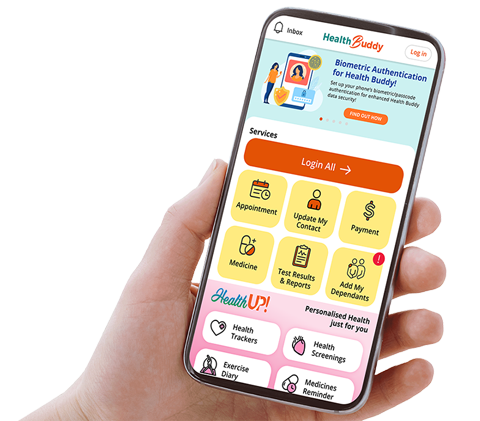
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.