Overview
The Myopia Research Group at Singapore Eye Research Institute (SERI), in conjunction with the Singapore National Eye Centre (SNEC) and National University of Singapore (NUS), has been involved in various aspects of myopia research over the last 20 years. Our group’s research focuses on five sub-themes: genetics, animal experimental models, epidemiology and community-based interventions, treatments to retard myopia progression and visually disabling pathologic myopia.
In our group, we aim to better understand the epidemiology, genetics, pathogenesis and public health implications of myopia and to develop and evaluate novel interventions to prevent or slow its progression in young children. We also focus on formulating better management strategies for myopia-related complications in older adulthood. Our multi-disciplinary team will address key questions to tackle the epidemic of myopia.
Projects
The Epidemiology Studies
Several large population-based studies have helped determine the prevalence of myopia in children, including the Singapore Cohort of Risk factors for Myopia (SCORM), which followed children aged 7-9 years for a period of 20 years, and the Strabismus Amblyopia and Refractive Error Singaporean preschool children (STARS), a cross-sectional study of children aged six months to six years. Data is also available from several adult studies, including the Singapore Malay, Indian and Chinese eye studies (SiMES, SINDI, SCES) which provide information of myopic prevalence in Singaporeans aged above 40 years. Early life data is also available from the GUSTO birth cohort involving 1,200 children where their refractive status was measured when they were 3, 6 and 9 years old.
From a combination of these studies, we know that 10% of children will be myopic by 5 years old, 60% by 12 years old and 80% by 18 years old. 20% of our young adult myopes will have high myopia which put them at greater risk of visual complications later on in life.
GUSTO light / FitSight study
One of the most important modifiable environmental risk factors for myopia is the lack of time outdoors in children. However, the biological mechanisms linking time outdoors and myopia in children remain poorly understood.
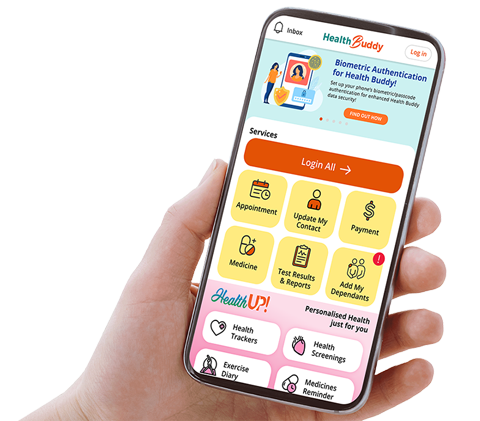
To address these gaps, we develop a novel FitSight watch to understand the effects of outdoor light exposure patterns on myopia. The FitSight watch was designed to continuously track and quantify light levels, the duration, timing and frequency of light exposure. Additionally, an activity diary was used to profile common outdoor activity types of children.
The FitSight watch was used in the Growing Up In Singapore Towards Healthy Outcomes (GUSTO) cohort study, comprising children who were delivered in two major tertiary hospitals in Singapore National University Hospital (NUH) and KK Women’s and Children’s Hospital (KKH). These children have been followed up yearly since birth. Myopia measurements of these children were taken at their 6th and 9th year visit. The FitSight watch and activity diaries were initially piloted among 367 children. A new and improved prototype of the FitSight watch was subsequently developed. Our FitSight watches and activity diaries were distributed to 698 myopic and non-myopic children at their 9th year visit, to evaluate light exposure patterns and outdoor activity types. Cycloplegic autorefraction and axial length (AL) were measured.
In our 9th year study, we found that children aged 9 years in Singapore have low time outdoors and light levels, spending 76% of their time outdoors in moderate light levels (<5000 lux). Increasing the duration spent outdoors, but not light levels or specific light exposure patterns, was protective against myopia.
Thus, our findings show that majority of time we spend outdoors at moderate outdoor light levels, and that increasing time outdoors even at these levels protect us from myopia. We recommend that children have 2 hours of outdoor activity per day starting from pre-school onwards.
SEED-High Myopia Study
The rate of high myopia is linked to the prevalence of myopia. Adults with high myopia (SE worse than -5.0 D) may have pathologic myopia (PM) complications that could result in visual impairment. The SEED High Myopia (SEED-HM) study aims to determine the 10-year changes in PM and its effects on visual function and health-related quality of life in adults with high myopia. The SEED older adult cohort comprises of 700 highly myopic adults from 4 Singapore studies: SP2, SiMES, SINDI, and SCES, while there are 123 from the SCORM young adult cohort. The adults will be recalled to the SERI clinic in 10 years and the fundus photographs/OCT will be graded for all PM lesions. Some of the tests performed include visual acuity (VA) for distance, biometry measurements, and fundus photographs.
We will also assess eye shape, choroidal thickness and choroidal vasculature using novel SS-OCT Angiogram imaging approaches and scleral rigidity with a novel adaption of B-scan ultrasound machine to compare high myopia with and without PM. The changing natural history of progression from high myopia to PM across age groups and generations in SEED and SCORM will provide valuable information on early and late predictors of PM. Wide-field OCT prototype can detect staphylomas in high myopes in SEED and high myopes in SEED with myopic macular degeneration have visual field defects different from glaucoma.
We have identified the risk factors for MMD amongst adults with high myopia and documented differences in visual field patterns for MMD, as well as increased risks of myopic traction maculopathy (MTM).
Our SEED-HM study will determine the 10-year changes in PM and effects on visual function and health-related quality of life in adults with high myopia and PM. Our proposal offers a new means of characterising disease phenotypes in PM, detailed evaluations of the impact on quality of life and new knowledge on imaging biomarkers that will provide baseline data for the development of new clinical treatments.
Fundus photographs based on the International Classification of Myopia Maculopathy in SEED-HM study
Together, these studies provide us with great detail of the size of the myopic problem in Singapore, and an opportunity to study risk factors associated with myopia.
Myopia and Genetics
Genetic studies in myopia show a complex interaction of multiple genetic influences. Our work with the international Consortium for Refractive Errors and Myopia (CREAM) has uncovered several novel genetics variants by meta-analysing genome-wide association studies (GWAS) from more than 30 population-based studies in Europe, Asia, the United States and Australia. The challenge now is to consolidate information to see if we can identify high risk children with genetic susceptibility for extreme myopia within the Singaporean Chinese population who will benefit from early interventions to slow down the progression of myopia.
Over the years, we have also studied the factors that influence myopia in our mouse and chick models. Our studies show that atropine reduces myopia progression in both pigmented and non-pigmented mice eyes. Atropine may also act on one or more muscarinic receptors to differentially regulate expression levels of specific receptors which in turn influence axial length and vitreous depth, the main morphological parameters associated with myopia.
Our muscarinic receptor knockout mouse study has provided in vivo evidence to support an important role for the M2/M3 muscarinic receptor in myopia development. The data indicates that the actions of the M2 receptor are mediated by changes in the expression of key extracellular matrix proteins, linking the functional role of M2 with scleral remodelling in myopia. The study also highlights the utility of the mouse as a model for myopia, particularly in conjunction with our new technologies that can measure ocular dimensions and optical properties with high precision. Further mouse studies are needed to pinpoint and validate the downstream targets of M2, as well as to investigate the role of the M3 receptor subtype in myopia development.
We now know that there is good potential for light-based interventions for myopia control. In our past chick models, we were able to show that manipulation of the chromaticity of light can also influence myopia progression. Chicks raised in red/green environment become more myopic, while those in blue/green light became more hyperopic. The next challenge is to determine if manipulation of lights similar/difference wavelengths or intensity could also slow myopic progression in non-human primate models and in children.
Recently, our researchers led by Dr Raymond Najjar and Assoc Prof Amutha Barathi in collaboration with the Visual Neurosciences Research Group and the Pre-clinical Translational Research Platform, have developed a state of the art research facility for evaluating the impact of light (intensity, spectrum, timing and duration) on different animal models including non-human primate (NHP). The NHP model includes Rhesus and Cynomolgus Macaques and was successfully developed in collaboration with Prof Earl Smith and Dr Li-Fang Hung (University of Houston, USA) using custom-built 3D-printed helmets equipped unilaterally with a Bangerter occlusion foil. We are currently using this model to evaluate the chronic impact of intermittent high intensity light exposures on ocular growth, myopia development and ocular vasculature and structure using swept-source optical coherence tomography-angiography (SS-OCT A) (Plex Elite 9000, Zeiss). Intermittent exposure to high intensity light is showing promising results in preventing the onset of myopia in NHPs. The team is also investigating 1/ the synergetic impact of defocus interruption and high intensity light (Biswas et al. 2021 — ARVO) and 2/ the impact of spectrally tailored indoor lighting strategies (Najjar et al. 2021 Sci Rep, Muralidharan et al. 2020 — ARVO) on emmetropization and ocular growth and metabolomics in chicken models of form-deprivation and lens-induced myopia. The ultimate goal of the group is to translate findings in the NHP and chicken models into feasible light therapy strategies for myopia prevention.
Interventional Studies: Slowing, Stopping and Reversing Myopia in Children
Researchers at SERI/SNEC have been exploring ways of slowing or stopping myopia using optical (e.g. progressive add, bifocal and myopic defocus glasses) and pharmacological (e.g. pirenzepine and atropine) interventions. Of these, results from the Atropine Treatment of Myopia (ATOM) studies have been most promising.
a. Atropine studies
There are two major ATOM studies, ATOM1 and ATOM2, involving a total of 800 subjects and testing a variety of doses of atropine over a three-to-five-year periods. In the ATOM1 study, we found that high doses of atropine (1.0%) can slow myopia over 2 years by 80%. However, care needed to be taken when stopping drops because of potential rebound. In the ATOM2 studies, it was noted that even very low doses of atropine (0.01%) could slow myopia progression by 50-60% with minimal to no side effects.
This has translated into clinical practice with many clinicians locally and worldwide now converting to lower doses. More work still needs to be done to better understand the exact pharmacological mechanism of the medication, and to tailor the treatment regime to each individual child. Low-dose atropine, however, has been one of the more exciting new developments in myopia management for some time.
In our on-going ATOM3 study, we hope to look to see if we could use low dose atropine to prevent onset of myopia and slow myopia progression in high-risk children who are not yet myopic or have very low myopia.
In the continuing journey, we plan to continue to study effect of different doses with the recent APPLE study (completed 2020) and combination of atropine and other treatment modalities (e.g. day-time multifocal contact lenses and myopia control glasses).
With regards to other pharmacological agents, in the 1990s, SERI also participated in a multi-centred study looking at the effect of a more selective drug, pirenzipine. However, the medication appeared less effective than atropine. We continue to look for novel candidates along the myopia-biopathway that may help to limit myopia progression.
b. Optical corrections
In the late 1990s, researchers at SERI first explored the use of rigid contact lenses and progressive add glasses on myopic progression. However, results from these studies were not encouraging.
Since then, several other optical devices (multifocal contact lenses, orthokeratoplasty and peripheral defocus glasses with lenslet design) which have been shown to also slow myopia progression. We continue to engage with the various industry partners to explore efficacy of these agents (either on its own or in combination with atropine). We are currently participating in a multi-centred multifocal contact lens study and have plans for future combination studies.
We acknowledge the assistance we have had over the years from the National Medical Research Council (NMRC) and Singapore Clinical Research Institute (SCRI); and also, our industry partners (such as Santen Pharmaceuticals and Johnson-Johnson Vision) who have provided us with support for these clinical studies.
c. Environmental
We also know that environmental factors, such as a lack of outdoor activity, may influence myopia onset and progression. Reasons for this are uncertain, but it is believed that levels of light intensity, chromatics and frequency may be important. The FIT outdoor trial evaluated a weekend park outdoor programme. There was a significant increase in mean outdoor time during the intervention “weekend park programme” (14.75 hours/week) compared with the control (12.40 hours/week). Besides, a novel fitness tracker (FitSight) has been developed to record light levels and encourage children to increase time they spend outdoors.
The tracker was evaluated in the FitSight study of 23 children, STARS study of 80 children and pilot GUSTO study of 367 children. The data of outdoor activity was collected using a one-week outdoor activity diary. Interestingly, children in Singapore go outdoors in episodes or spurts of about 20 minutes six to eight times per day. The top outdoor activities from the diaries were walking, playing at a park and running for younger children. For teenage children, the top outdoor activities were walking, running and ball games.
The light data from Fitsight watch had provided valuable information on the development of outdoor programs in different settings, such as school and communities. Our proposed outdoor physical activity programme will be integrated into schools and rolled out nationwide in conjunction with the Ministries of Education and Health (Health Promotion Board).
Myopia, HM rates and associated visual impairment have been reduced in the population of Singapore by increasing outdoor time for children and preventing or delaying early-onset of myopia. Steps have been made to undertake an exploratory randomised controlled study both locally and in conjunction with collaborators overseas. Combined outdoor preventive measures and myopia treatment control are expected to be beneficial with added additive efficacy.
Clinical Myopia Cohorts — Pathologies related to High Myopia
To better understand the progression of myopia over time, we have set up 3 myopia cohorts consisting of children, myopic adults without pathology and myopic adults with pathology.
This set of research projects aims to prevent or delay the onset of childhood myopia, minimise the subsequent impact on quality-of-life and quality-of-vision in adulthood (e.g. through optical and surgical correction) and mitigate any myopia-related complications which may occur in mid-to-late adulthood.
Locally, the myopic epidemic started in the 1980s, with a prevalence of high myopia of 20 to 30% of individuals from that generation of Singaporeans are now entering their 5th decade where myopic complications (such as glaucoma, pathological myopia, retinal detachment, macula neovascularisation and, early cataracts) are likely to start manifesting.
To better understand the progression of myopia over time, we have set up 3 myopia cohorts consisting of children, myopic adults without pathology and myopic adults with pathology.
Myopic Adults with and without Pathology
Pathologic Myopia (PM) is the most severe form of myopia, in which sight-threatening complications are common and potentially blinding. About 2 to 15 out of every 1,000 people suffer from vision impairment due to pathological myopia in Asia.
To date, it still remains unclear whether high myopia can eventually develop into pathological myopia. In our adult Myopic and Pathologic Eyes in Singapore (MyoPES) clinic where we provide clinical eye care services to these patients with high myopia - particularly those who are of highest risk of developing pathological myopia - our ongoing research studies led by Assoc Prof Donny Hoang and Dr Wong Chee Wai, coupled with the use of recent advances in imaging technology aim to uncover the underlying mechanisms that contribute to pathological myopia and the development of new treatment options that could resolve this public health concern.
Prospective Clinic Based Cohort Study of High Myopia and Pathologic Myopia (PROMPT) Study
Our PROMPT study aims to evaluate prospective ocular imaging in adults with highly myopic eyes (including both pathologic (with staphyloma and/or myopic macular degeneration) and non-pathologic eyes), in order to integrate any new findings across novel ways of using routine and innovative imaging modalities such as optical coherence tomographic angiography (OCTA), enabling detailed in vivo study of the changes in the choroid associated with PM. Additionally, ocular tissue samples, normally acquired in surgery and discarded, are preserved and analysed, which may offer new insights into disease pathogenesis, improve risk stratification and reveal novel therapeutic targets for the treatment of the various complications of high myopia.
We found that macular function in adult highly myopic eyes using Microperimeter (MP-3) and observed the strong correlation with increasing axial length (AL), poorer best corrected visual acuity (BCVA) and the worsening severity of myopic macular degeneration (MMD) (Wong et al, ARVO. 2020). Similarly, this was identified by Yu et al (ARVO 2020) where high myopic eyes with longer AL ≥29.5 mm have a higher prevalence of myopic traction maculopathy related complications such as foveoschisis and vitreomacular traction as compared to shorter eyes (AL < 29.5 mm).
Most recently, our team further investigated the pathogenesis of early vision impairment in high myopic eyes by integrating functional and structural parameters such as macular function and OCTA (Plex Elite), possibly innovating the clinical use in monitoring MMD progression.
The Scleral Biomechanical Properties in Pathologic Myopia and Myopic Glaucoma (PMG) Study
With various population-based epidemiological studies suggesting the strong association between myopia and the development of glaucoma, the consequence of the resultant axial elongation in highly myopic eyes remains uncertain. Our PMG study is prospective ocular imaging study of myopic patients (low myopia, high myopia, extremely high myopia and pathologic myopia) and myopic-glaucoma patients aims to incorporate established and advanced imaging technologies such as OCT coupled with ophthalmodynametry, ultrawide-field OCT, ultrasound elastography and in select patients, magnetic resonance imaging (MRI) that enable detailed in vivo examination of stress-strain relationships in the posterior sclera associated with PM. These new and insightful findings may be revealed with multimodal imaging that will further understanding of disease pathways in high and pathologic myopia, and the link between glaucoma and myopia.
Our preliminary reports have shown that high myopia (HM) eyes tend to be more sensitive to intraocular pressure (IOP) elevation as compared to low myopia (LM) eyes. Moreover, pathologic myopia (PM) eyes experienced abnormally high strains and they were equally influenced by IOP elevation and adduction (turning of the eye in toward the nose, a movement required for near work and reading). This may indicate that optic nerve head (ONH) strain differs significantly between LM, HM and PM eyes and has the potential to serve as a biomarker for progression (Hoang, et al, ARVO. 2020).
Recently, we have assessed the changes in the posterior eye shape in these eyes by using Ultrasound elastography (20-MHz Ultrasound), especially in eyes with and without the presence of staphyloma (local outpouching in posterior eye wall), we discovered obvious morphological changes in PM eyes as compared to other groups (LM and HM eyes). Along with the in vivo examination using sequential external pressure application, this could serve as a potential method of assessing the eye wall mechanism properties during the deformation that occurs in the progression of pathological myopia (Ito et al, IEEE. 2020).
In our collaboration with Columbia University (New York City, USA) in an MRI imaging study in highly myopic eyes with the presence of staphyloma further supported the phenomenon of gaze-induced globe deformation was noted in all gazes, but most importantly reversible, instantaneous axial length increase in the vitreous chamber occurred only in downgaze, which is consistent with studies supporting the association of environmental factors such as near work with myopia development and progression (Hoang et al, BJO. 2020). In the most recent works, we have developed an algorithm for the detection of staphyloma using ultrasound elastography, which may allow for ultrasound operators who are not clinically trained (people who are neither ophthalmologists nor optometrists) to be able to detect staphyloma (Hoang et al, ARVO 2021).
Novel Therapies for High and Pathologic Myopia
Based on our clinical studies, we hypothesise that a less stiff and more deformable eye wall is more prone toward the development and progression of pathologic myopia. In people, this goal is achieved by utilising imaging modalities such as optical coherence tomography, magnetic resonance imaging and novel high-resolution, high-frequency ultrasonography (and other optical photoacoustic systems) of the eye at rest and during biomechanical stress-strain stimuli.
Concurrent work lead by Assoc Prof Donny Hoang, in collaboration with the Ocular Imaging Department and the University of Newcastle, Australia and Riverside Research Institute, in New York, USA, utilises a guinea pig animal model of high myopia with staphyloma to advance imaging modalities (such as acoustic microscopy and quantitative ultrasonography, Hoang et al. Exp Eye Res. 2019) that may predict which eyes will progress to pathology and to direct treatment to allow for personalised medicine. Work in the Hoang lab also explores novel therapeutic approaches in animal models where non-light-activated chemicals are applied in vivo to crosslink the collagen in eye walls to act as a mortar, stiffening the wall and stunting eye elongation (and progression of near-sightedness). Our work has demonstrated that a single injection of our chemical results in about half the amount of refractive error that would occur in growing guinea pigs (approximately -6 dioptres) and can also stunt the development of experimentally-induced myopia as well (Hoang and McFadden, ARVO 2019).
Directions of Myopia Research
This first challenge in myopia research is to understand the myopia process. Our epidemiology, genetic and animal studies have come a long way. We now understand the size and impact of myopia in our population, the risk associations which drive myopia progression in childhood, and a gradual understanding of the genetic and biological processes that cause myopia. There is, however, still much to learn. We still do not fully understand how genetics and environmental factors interact, what changes are occurring on a biological level which stimulate and inhibit the myopia process, and whether there are novel genetic/pharmaceutical targets we can use to modify this process.
Clinically, we continue to explore measures to prevent onset of myopia and progression in childhood. Many Asian countries now have national programs which promote changes in behaviour (spending time outdoors). However, this is often not enough. Fortunately, there are now also several pharmacological and optical treatments to control myopia. The challenge now is to continue to assess these and other novel interventions (individually and in combinations), and to develop treatment strategies targeted to individual risk profiles.
Lastly, it is also important to prevent complication and visual loss in adults with high myopia. If we cannot prevent myopia, then can we prevent visual loss from its complications. It is hoped through our cohort studies, we can better identify individuals most at risk, to develop timely interventions to delay/prevent onset of complications, and better treatments for these complications.
Publications
Epidemiological/cohort studies
- Saw SM, Katz J, Schein OD, Chew SJ, Chan TK. Epidemiology of myopia. Epidemiol Rev. 1996;18(2):175-87. Doi: 10.1093/oxfordjournals.epirev.a017924.
- Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012; 379(9827):1739-48.
- Saw SM, Matsumura S, Hoang QV. Prevention and management of myopia and myopic pathology. Invest Ophthalmol Vis Sci. 2019 Feb 1;60(2):488-499.
- Matsumura S, Cheng CY, Saw SM. Global epidemiology of myopia (Book Chapter). Updates on Myopia. 2019 Oct;27-51. doi: 10.1007/978-981-13-8491-2_2.
- Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw SM. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020 Jan 14;20(1):27.
- Saw SM, Tong L, Chua WH, Koh D, Tan DTH, Katz J. Incidence and progression of myopia in Singapore school children. Invest Ophthalmol. Vis Sci. 2005; 46:51-57.
- Matsumura S, Lanca C, Htoon HM, Brennan N, Tan CS, Kathrani B, Chia A, Tan D, Sabanayagam C, Saw SM. Annual myopia progression and subsequent 2-year myopia progression in Singaporean children. Transl Vis Sci Technol. 2020 Dec 7;9(13):12.
- Li J, Lanca C, Htoon HM, Wong YL, Nyunt SZ, Tan D, Sabanayagam C, Saw SM. High myopes in Singapore: 19-year progression from childhood to adulthood. Ophthalmology. 2020 Dec;127(12):1768-1770. doi: 10.1016/j.ophtha.2020.05.031.
- Saw SM, Hong CY, Chia KS, Stone RA, Tan D. Nearwork and myopia in young children. Lancet. 2001 Feb 3;357(9253):390. doi: 10.1016/S0140-6736(05)71520-8.
- Chong YS, Liang Y, Gazzard G, Stone RA, Saw SM. Association between breastfeeding and likelihood of myopia in children. JAMA Journal of the American Medical Association. 2005; 293:3001-2.
- Low W, Dirani M, Gazzard G, Chan YH, Zhou HJ, Selvaraj P, Au Eong KG, Young TL, Mitchell P, Wong TY, Saw SM. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol. 2010;94(8):1012-6.
- Lanca C, Saw SM. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol Opt. 2020 Mar;40(2):216-229.
- Jiang X, Tarczy-Hornoch K, Cotter SA, Matsumura S, Mitchell P, Rose KA, Katz J, Saw SM, Varma R, POPEYE Consortium. Association of parental myopia with higher risk of myopia among multiethnic children before school age. JAMA Ophthalmol. 2020 May 1;138(5):501-509.
- Samarawickrama C, Mitchell P, Tong L, Gazzard G, Lim L, Wong TY, Saw SM. Myopia-related optic disc and retinal changes in adolescent children from Singapore. Ophthalmol. 2011; 118:2050-7.
- Wong YL, Ding Y, Sabanayagam C, Wong CW, Verkicharla P, Ohno-Matsui K, Tan D, Yeo AC, Hoang QV, Lamoureux E, Saw SM. Longitudinal changes in disc and retinal lesions among highly myopic adolescents in Singapore over a 10-year period. Eye Contact Lens. 2018 Sep;44(5):286-291. doi: 10.1097/ICL.0000000000000466.
- Matsumura S, Kuo AN, Saw SM. An update of eye shape and myopia. Eye Contact Lens. 2019 Sep;45(5):279-285.
- Ang M, Wong CW, Hoang QV, Cheung GCM, Lee SY, Chia A, Saw SM, Ohno-Matsui K, Schmetterer L. Imaging in myopia: Potential biomarkers, current challenges and future developments. Br J Ophthalmol. 2019 Jun;103(6):855-862.
Genetic
- Fan Q, Zhou X, Khor CC, Cheng CY, Goh LK, Sim X, Tay WT, Li YJ, Ong RT, Suo C, Cornes B, Ikram MK, Chia KS, Seielstad M, Liu J, Vithana E, Young TL, Tai ES, Wong TY, Aung T, Teo YY, Saw SM. Genome-wide meta-analysis of five Asian cohorts identifies PDGFRA as a susceptibility locus for corneal astigmatism. PLoS Genet. 2011; 7(12): e1002402.
- Seow WJ, Ngo CS, Pan H, Barathi VA, Tompson SW, Whisenhunt KN, Vithana E, Chong YS, Juo SH, Hysi P, Young TL, Karnani N, Saw SM. In-utero epigenetic factors are associated with early-onset myopia in young children. PLoS One. 2019 May 17;14(5): e0214791. doi: 10.1371/journal.pone.0214791. PMID: 31100065; PMCID: PMC6524791.
- Wong YL, Hysi P, Cheung G, Tedja M, Hoang QV, Tompson SWJ, Whisenhunt KN, Verhoeven V, Zhao W, Hess M, Wong CW, Kifley A, Hosoda Y, Haarman AEG, Hopf S, Laspas P, Sensaki S, Sim X, Miyake M, Tsujikawa A, Lamoureux E, Ohno-Matsui K, Nickels S, Mitchell P, Wong TY, Wang JJ, Hammond CJ, Barathi VA, Cheng CY, Yamashiro K, Young TL, Klaver CCW, Saw SM, Consortium of Refractive Error, Myopia (CREAM). Genetic variants linked to myopic macular degeneration in persons with high myopia: CREAM Consortium. PLoS One. 2019 Aug 15;14(8): e0220143. doi: 10.1371/journal.pone.0220143. Erratum in: PLoS One. 2019 Oct 10;14(10): e0223942. PMID: 31415580; PMCID: PMC6695159.
- Wong YL, Hysi P, Cheung G, Tedja M, Hoang QV, Tompson SWJ, Whisenhunt KN, Verhoeven VJM, Zhao W, Hess M, Wong CW, Kifley A, Hosoda Y, Haarman AEG, Hopf S, Laspas P, Sensaki S, Sim X, Miyake M, Tsujikawa A, Lamoureux E, Ohno-Matsui K, Nickels S, Mitchell P, Wong TY, Wang JJ, Hammond CJ, Barathi VA, Cheng CY, Yamashiro K, Young TL, Klaver CCW, Saw SM, Consortium of Refractive Error, Myopia (CREAM). Correction: Genetic variants linked to myopic macular degeneration in persons with high myopia: CREAM Consortium. PLoS One. 2019 Oct 10;14(10): e0223942. doi: 10.1371/journal.pone.0223942. Erratum for: PLoS One. 2019 Aug 15;14(8): e0220143. PMID: 31600355; PMCID: PMC6786527.
- Fan Q, Pozarickij A, Tan NYQ, Guo X, Verhoeven VJM, Vitart V, Guggenheim JA, Miyake M, Tideman JWL, Khawaja AP, Zhang L, MacGregor S, Höhn R, Chen P, Biino G, Wedenoja J, Saffari SE, Tedja MS, Xie J, Lanca C, Wang YX, Sahebjada S, Mazur J, Mirshahi A, Martin NG, Yazar S, Pennell CE, Yap M, Haarman AEG, Enthoven CA, Polling J; Consortium for Refractive Error and Myopia (CREAM); UK Biobank Eye and Vision Consortium, Hewitt AW, Jaddoe VWV, van Duijn CM, Hayward C, Polasek O, Tai ES, Yoshikatsu H, Hysi PG, Young TL, Tsujikawa A, Wang JJ, Mitchell P, Pfeiffer N, Pärssinen O, Foster PJ, Fossarello M, Yip SP, Williams C, Hammond CJ, Jonas JB, He M, Mackey DA, Wong TY, Klaver CCW, Saw SM, Baird PN, Cheng CY. Genome-wide association meta-analysis of corneal curvature identifies novel loci and shared genetic influences across axial length and refractive error. Commun Biol. 2020 Mar 19;3(1):133. doi: 10.1038/s42003-020-0802-y. PMID: 32193507; PMCID: PMC7081241.
Animal studies
- Lim W, Kwan JL, Goh LK, Beuerman RW, Barathi VA. Evaluation of gene expression profiles and pathways underlying postnatal development in mouse sclera. Mol Vis. 2012; 18:1436-48.
- Barathi VA, Weon SR, Tan QS, Lin KJ, Tong L, Beuerman RW. Transglutaminases (TGs) in ocular and periocular tissues: Effect of muscarinic agents on TGs in scleral fibroblasts. PLoS One. 2011;6(4): e18326.
- Rozema J, Dankert S, Iribarren R, Lanca C, Saw SM. Axial growth and lens power loss at myopia onset in Singaporean children. Invest Ophthalmol Vis Sci. 2019 Jul 1;60(8):3091-3099. doi: 10.1167/iovs.18-26247. PMID: 31323091.
- Barathi VA, Beuerman RW. Molecular mechanisms of muscarinic receptors in mouse scleral fibroblasts: Prior to and after induction of experimental myopia with atropine treatment. Mol Vis. 2011;17:680-92.
- Hoang QV, Rohrbach D, McFadden SA, Mamou J. Regional changes in the elastic properties of myopic Guinea pig sclera. Exp Eye Res. 2019 Sep;186:107739.
- Najjar RP, Chao De La Barca JM, Barathi VA, et al. Ocular growth and metabolomics are dependent upon the spectral content of ambient white light. Scientific Reports. 2021;11(1):7586. doi:10.1038/s41598-021-87201-2..
Childhood intervention studies
- Katz J, Schein OD, Levy B, Cruiscullo T, Saw SM, Rajan U, Chan TK, Yew Khoo C, Chew SJ. A randomized trial of rigid gas permeable contact lenses to reduce progression of children's myopia. Am J Ophthalmol. 2003 Jul;136(1):82-90.
- Tan DT, Lam DS, Chua WH, Shu-Ping DF, Crockett RS, Asian Pirenzepine Study Group. One-year multicenter, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. Ophthalmology. 2005 Jan;112(1):84-91.
- Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, Tan D. Atropine for the treatment of childhood myopia. Ophthalmology. 2006 Dec; 113(12):2285-91.
- Tong L, Huang XL, Koh AL, Zhang X, Tan DT, Chua WH. Atropine for the treatment of childhood myopia: Effect on myopia progression after cessation of atropine. Ophthalmology 2009 Mar;116(3):572-9. Epub 2009 Jan 22.
- Chia A, Chua WH, Tan D. Effect of topical atropine on astigmatism. Br J Ophthalmol. 2009 Jun;93(6):799-802.
- Loh KL, Lu Q, Tan D, Chia A. Risk factors for progressive myopia in atropine therapy for myopia (ATOM1 study). Am J Ophthalmol. Mar 2015; 159(5):945-9
- Luu CD, Lau AM, Koh AH, Tan D. Multifocal electroretinogram in children on atropine treatment for myopia. Br J Ophthalmol. 2005 Feb;89(2):151-3.
- Kumaran A, Htoon MH, Tan D, Chia A. Analysis of changes in refraction and biometric parameters in atropine and placebo treated eyes. IOVS Aug 2015; 56(9): 5650-5.
- Chia A, Li W, Tan D, Luu CD. Full-field electroretinogram findings in children in the atropine treatment for myopia (ATOM2) study. Doc Ophthalmol. 2013 Jun;126(3):177-86. doi: 10.1007/s10633-012-9372-8.
- Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, Tan D. Atropine for the treatment of childhood myopia: Safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119(2):347-54.
- Chia A, Li W, Chua WH, Goon YY, Fong A, Tan D. Changes after cessation of atropine: ATOM2. Am J Ophthalmol. 2014 Feb; 157(2): 451-7.
- Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: Myopia control with 0.01% eyedrops. Ophthalmology. 2016 Feb;123(2):391-9.
- Verkicharla PK, Ramamurthy D, Nguyen QD, Zhang X, Pu SH, Malhotra R, Ostbye T, Lamoureux EL, Saw SM. Development of the fitsight fitness tracker to increase time outdoors to prevent myopia. Transl Vis Sci Technol. 2017 Jun 16;6(3):20. doi: 10.1167/tvst.6.3.20. eCollection 2017 Jun.
- Lanca C, Teo A, Vivagandan A, Htoon HM, Najjar RP, Spiegel DP, Pu SH, Saw SM. The effects of different outdoor environments, sunglasses and hats on light levels: Implications for myopia prevention. Transl Vis Sci Technol. 2019 Jul 18;8(4):7. doi: 10.1167/tvst.8.4.7. PMID: 31360613; PMCID: PMC6656201.
- Wildsoet CF, Chia A, Cho P, Guggenheim JA, Polling JR, Read S, Sankaridurg P, Saw SM, Trier K, Walline JJ, Wu PC, Wolffsohn JS. IMI - Interventions Myopia Institute: Interventions for controlling myopia onset and progression report. Invest Ophthalmol Vis Sci. 2019 Feb 28;60(3):M106-M131. doi: 10.1167/iovs.18-25958. Erratum in: Invest Ophthalmol Vis Sci. 2019 Apr 1;60(5):1768. PMID: 30817829.
- Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith Iii EL, Zhou X, Matsui KO, Wu PC, Sankaridurg P, Chia A, Rosman M, Lamoureux EL, Man R, He M. Myopia. Nat Rev Dis Primers. 2020 Dec 17;6(1):99. doi: 10.1038/s41572-020-00231-4. PMID: 33328468.
- Wong CW, Foo LL, Morjaria P, Morgan I, Mueller A, Davis A, Keys D, He M, Sankaridurg P, Zhu JF, Hendicott P, Tan D, Saw SM, Cheng CY, Lamoureux EL, Crowston JG, Gemmy Cheung CM, Sng C, Chan C, Wong D, Lee SY, Agrawal R, Hoang QV, Su X, Koh A, Ngo C, Chen H, Wu PC, Chia A, Jonas JB, Wong TY, Ang M. Highlights from the 2019 International Myopia Summit on 'controversies in myopia'. Br J Ophthalmol. 2020 Aug 18: bjophthalmol-2020-316475. doi: 10.1136/bjophthalmol-2020-316475. Online ahead of print. PMID: 32816799.
Adult high myopia
- Wong YL, Sabanayagam C, Ding Y, Wong CW, Yeo AC, Cheung YB, Cheung G, Chia A, Ohno-Matsui K, Wong TY, Wang JJ, Cheng CY, Hoang QV, Lamoureux E, Saw SM. Prevalence, risk factors, and impact of myopic macular degeneration on visual impairment and functioning among adults in Singapore. Invest Ophthalmol. Vis Sci. 2018 Sep 4;59(11):4603-4613. doi: 10.1167/iovs.18-24032.
- Devarajan K, Sim R, Chua J, Wong CW, Matsumura S, Htoon HM, Schmetterer L, Saw SM, Ang M. Optical coherence tomography angiography for the assessment of choroidal vasculature in high myopia. Br J Ophthalmol. 2020 Jul;104(7):917-923. doi: 10.1136/bjophthalmol-2019-314769. Epub 2019 Oct 4. PMID: 31585963.
- Cahyo DAY, Wong DWK, Yow AP, Saw SM, Schmetterer L. Volumetric choroidal segmentation using sequential deep learning approach in high myopia subjects. Annu Int Conf IEEE Eng Med Biol Soc. 2020 Jul; 2020:1286-1289. doi: 10.1109/EMBC44109.2020.9176184. PMID: 33018223.
- Lim LS, Matsumura S, Htoon HM, Tian J, Lim SB, Sensaki S, Chen C, Hilal S, Wong TY, Cheng CY, Kuo A, Saw SM. MRI of posterior eye shape and its associations with myopia and ethnicity. Br J Ophthalmol. 2020 Sep;104(9):1239-1245. doi: 10.1136/bjophthalmol-2019-315020. Epub 2019 Dec 2. PMID: 31791940.
- Matsumura S, Sabanayagam C, Wong CW, Tan CS, Kuo A, Wong YL, Ohno-Matsui K, Wong TY, Cheng CY, Hoang QV, Saw SM. Characteristics of myopic traction maculopathy in myopic Singaporean adults. Br J Ophthalmol. 2021 Apr;105(4):531-537. doi: 10.1136/bjophthalmol-2020-316182. Epub 2020 May 23. PMID: 32447325.
- Wong YL, Sabanayagam C, Wong CW, Cheung YB, Man REK, Yeo AC, Cheung G, Chia A, Kuo A, Ang M, Ohno-Matsui K, Wong TY, Wang JJ, Cheng CY, Hoang QV, Lamoureux E, Saw SM. Six-year changes in myopic macular degeneration in adults of the Singapore epidemiology of eye diseases study. Invest Ophthalmol Vis Sci. 2020 Apr 9;61(4):14. doi: 10.1167/iovs.61.4.14. PMID: 32298432; PMCID: PMC7401489.
- Zheng F, Wong CW, Sabanayagam C, Cheung YB, Matsumura S, Chua J, Man REK, Ohno-Matsui K, Wong TY, Cheng CY, Tai ES, Lamoureux ELED, Schmetterer L, Kuo A, Hoang QV, Saw SM. Prevalence, risk factors and impact of posterior staphyloma diagnosed from wide-field optical coherence tomography in Singapore adults with high myopia. Acta Ophthalmol. 2021 Mar;99(2): e144-e153. doi: 10.1111/aos.14527. Epub 2020 Jun 29. PMID: 32602252.
- Wong YL, Zhu X, Tham YC, Yam JCS, Zhang K, Sabanayagam C, Lanca C, Zhang X, Han SY, He W, Susvar P, Trivedi M, Yuan N, Lambat S, Raman R, Song SJ, Wang YX, Bikbov MM, Nangia V, Chen LJ, Wong TY, Lamoureux EL, Pang CP, Cheng CY, Lu Y, Jonas JB, Saw SM, Asian Eye Epidemiology Consortium (AEEC). Prevalence and predictors of myopic macular degeneration among Asian adults: \Pooled analysis from the Asian Eye Epidemiology Consortium. Br J Ophthalmol. 2020 Sep 2:bjophthalmol-2020-316648. doi: 10.1136/bjophthalmol-2020-316648. Online ahead of print. PMID: 32878826.
- Hoang QV, Chang S, Yu DJG, Yannuzzi LA, Freund KB and Grinband J. 3-D assessment of gaze-induced eye shape deformations and downgaze-induced vitreous chamber volume increase in highly myopic eyes with staphyloma. Br J Ophthalmol. 2020 Aug 23:bjophthalmol-2020-316084. doi: 10.1136/bjophthalmol-2020-316084. Online ahead of print.
- Sim SS, Wong CW, Hoang QV, Lee SY, Wong TY, Cheung CMG. Anti-retinal autoantibodies in myopic macular degeneration: A pilot study. Eye (Lond). 2020 Oct 28. doi: 10.1038/s41433-020-01241-y. Online ahead of print.
- Tey KY*, Wong QY, Dan YS, Tsai ASH, T DSW, Ang M, Cheung CMG, Lee SY, Wong TY, Hoang QV*, Wong CW. Association of aberrant posterior vitreous detachment and pathologic tractional forces with myopic macular degeneration. Invest Ophthalmol Vis Sci. 2020 Jun 1;62(7):7. doi: 10.1167/iovs.62.7.7.
- Zheng F, Chua J, Ke M, Tan B, Yu M, Hu Q, Cheung C, Ang M, Lee SY, Wong TY, Schmetterer, Wong CW, Hoang QV. Quantitative OCT Angiography of the retinal microvasculature and choriocapillaris in highly myopic eyes with myopic macular degeneration. Br J Ophthalmol. 2021 Jan 4:bjophthalmol-2020-317632. doi: 10.1136/bjophthalmol-2020-317632. Online ahead of print.
- Wang X, Chang S, Grinband J, Yannuzzi LA, Freund KB, Hoang QV*^, Girard MJ*. Optic nerve tortuosity and displacements during horizontal eye movements in healthy and highly myopic subjects. Br J Ophthalmol. 2021 May 26:bjophthalmol-2021-318968. doi: 10.1136/bjophthalmol-2021-318968.Online ahead of print.
Members
Head
- Prof Saw Seang Mei
- Assoc Prof Audrey Chia
Key Team Members
- Clin Prof Donald Tan
- Prof Wong Tien Yin
- Prof Cheng Ching-Yu
- Assoc Prof Veluchamy Amutha Barathi
- Dr Raymond Najjar
- Assoc Prof Marcus Ang
- Assoc Prof Donny Hoang Quan V.
- Dr Wong Chee Wai
- Dr Arumugam R Muralidharan
- Dr Foo Li Lian
- Dr Loh Kai-Lyn